Last updated on December 18th, 2024 at 03:27 am
- 1. The Nature of Bipolar Disorder
- 1.1 Types of Bipolar Disorder
- 1.2 Symptoms of Bipolar Episodes
- 2. The Intersection of Bipolar Disorder and Addiction
- 2.1 Statistical Overview
- 2.2 Bidirectional Relationship
- 3. Factors Contributing to Comorbidity
- 3.1 Genetic Predisposition
- 3.2 Neurobiological Factors
- 3.3 Self-Medication Hypothesis
- 3.4 Environmental Stressors
- 4. Challenges in Diagnosis
- 4.1 Overlapping Symptoms
- 4.2 Temporal Relationship
- 4.3 Screening and Assessment Tools
- 5. Treatment Approaches for Dual Diagnosis
- 5.1 Integrated Treatment Models
- 5.2 Pharmacological Interventions
- 5.3 Psychotherapeutic Approaches
- 5.4 Lifestyle Modifications
- 6. Challenges in Recovery
- 6.1 Medication Compliance
- 6.2 Relapse Prevention
- 6.3 Social and Occupational Functioning
- 7. Future Directions in Research and Treatment
- 7.1 Personalized Medicine Approaches
- 7.2 Novel Pharmacological Interventions
- 7.3 Technology-Assisted Interventions
- The Impact of Substance Use on Bipolar Disorder Patients
- Mixed Episodes and Co-occurring Substance Use
- Common Risk Factors and Dual Diagnosis Challenges
- Affective Episodes and Secondary Substance Dependency
- Treatment Approaches for Dual Diagnosis
- Therapeutic Interventions for Long-term Recovery
- Mental Health Dual Diagnosis and Social Functioning
- Factors for Addiction and Anxiety Disorders
- Addressing Personality Disorders and Affective Symptoms
- Impact of Behavioural Addictions on Bipolar Disorder
- Innovative Treatment Strategies and Dual Diagnosis Management
- Co-occurring Disorders and Major Depression
- Daily Life and Emotional Regulation
- Suicidal Ideations and Comorbid Addictions
- Bipolar Disorder Intervention Strategies
- Secondary Substance Dependency and Recovery Support
- Bipolar Disorder Substance Abuse Statistics and Prevalence Rates
- Comorbid Substance Use and Behavioral Addictions
- Depressive Disorders and Mixed Episodes
- Psychomotor Agitation in Bipolar Disorder
- Real Life Impacts of Dual Diagnosis
- Coping Strategies and Treatment Resources
- Addressing Stigma and Myths Surrounding Bipolar Disorder and Addiction
- StepRecovering from Addiction with Co-occurring Bipolar Disorder
- Integrated Treatment for Bipolar Disorder and Addiction
- Addressing Long-Term Recovery for Bipolar Patients
- Weight Gain as a Side Effect of Bipolar Disorder Medication
- Bipolar Diagnosis and Secondary Substance Dependency
- Prevalence of Comorbid Addictions in Bipolar Disorder
- Relationship Issues and Social Dynamics
- Substance Abuse Treatment and Medical Professional Involvement
- Addressing Affective Symptoms in Bipolar Addiction Comorbidity
- Major Depression and Depressive Disorders in Bipolar Patients
- Addiction Recovery Resources for Bipolar Disorder Patients
- Comorbidity in Alcohol Use and Bipolar Disorder
- Addressing Schizoaffective Disorders and Bipolar Disorder
- Illicit Drugs and Substance Use in Bipolar Disorder
- Bipolar Disorder and the Role of Aftercare Programmes
- Conclusion
- Frequently Asked Questions
- What Is The Relationship Between Bipolar Disorder And Addiction?
- Why Do Individuals With Bipolar Disorder Often Struggle With Alcohol Abuse?
- How Do Bipolar Disorder Symptoms Impact Substance Use?
- What Are Common Risk Factors For Dual Diagnosis Of Bipolar Disorder And Addiction?
- How Do Co-Occurring Disorders Affect Daily Life?
- How Does Cyclothymic Disorder Relate To Substance Use?
- What Treatment Options Are Available For Co-Occurring Bipolar Disorder And Addiction?
- How Do Mixed Episodes Complicate Addiction Treatment?
- What Is The Lifetime Prevalence Of Addiction Among Bipolar Patients?
- How Can Emotional Regulation Help In Managing Bipolar Disorder And Addiction?
- How Do Manic Periods Affect Substance Use?
- How Does Alcohol Use Disorder Exacerbate Bipolar Disorder Symptoms?
- What Is The Role Of Individual Therapy In Dual Diagnosis Treatment?
- How Does Substance Abuse Treatment Differ For Bipolar Disorder Patients?
- What Are The Detrimental Effects Of Drug Use On Bipolar Disorder?
- How Can Family Therapy Aid In Treating Bipolar Disorder And Addiction?
- What Challenges Arise In Treating Bipolar Addiction?
- How Do Mood Stabilizers Impact Substance Abuse In Bipolar Disorder?
- What Are Effective Strategies For Preventing Relapse In Bipolar Addiction?
- How Do Mixed Episodes Affect Social Skills And Relationships In Bipolar Patients?
Bipolar disorder and substance addiction often intertwine in complex ways, creating significant challenges for those affected and their loved ones. This intricate relationship between mood disorders and substance abuse requires careful examination to understand its origins, manifestations, and potential treatment approaches.
Let’s discover the connection between bipolar disorder and addiction, their shared triggers, and how tailored treatment plans can lead to better recovery outcomes.
1. The Nature of Bipolar Disorder
Bipolar disorder, formerly known as manic-depressive illness, is a chronic mental health condition characterized by extreme mood swings. These fluctuations range from manic or hypomanic episodes of elevated mood and energy to depressive episodes of profound sadness and lethargy.
1.1 Types of Bipolar Disorder
The mental health community recognizes several distinct types of bipolar disorder:
- Bipolar I Disorder: Characterized by manic episodes lasting at least seven days, or severe manic symptoms requiring immediate hospital care. Depressive episodes typically last at least two weeks.
- Bipolar II Disorder: Defined by a pattern of depressive and hypomanic episodes, but not the full-blown manic episodes seen in Bipolar I.
- Cyclothymic Disorder: A milder form of bipolar disorder, involving numerous periods of hypomanic and depressive symptoms lasting for at least two years.
1.2 Symptoms of Bipolar Episodes
Manic episodes may include:
- Increased energy and activity
- Excessively high, euphoric mood
- Irritability
- Racing thoughts and rapid speech
- Decreased need for sleep
- Poor judgment and impulsivity
Depressive episodes often involve:
- Persistent sad or empty mood
- Loss of interest in previously enjoyable activities
- Fatigue and decreased energy
- Difficulty concentrating and making decisions
- Changes in sleep patterns
- Thoughts of death or suicide
2. The Intersection of Bipolar Disorder and Addiction
The co-occurrence of bipolar disorder and substance addiction is alarmingly common. Research indicates that individuals with bipolar disorder are significantly more likely to develop substance use disorders compared to the general population.
2.1 Statistical Overview
Recent studies suggest that up to 60% of individuals with bipolar disorder will experience a substance use disorder at some point in their lives. This rate is substantially higher than the general population, where lifetime prevalence of substance use disorders is estimated at around 10-20%.
2.2 Bidirectional Relationship
The relationship between bipolar disorder and addiction is bidirectional, meaning each condition can influence and exacerbate the other. Substance abuse may trigger or worsen bipolar symptoms, while the mood swings associated with bipolar disorder can lead to self-medication with drugs or alcohol.
3. Factors Contributing to Comorbidity
Several factors contribute to the high rates of comorbidity between bipolar disorder and substance addiction:
3.1 Genetic Predisposition
Research suggests a shared genetic vulnerability for both bipolar disorder and addiction. Certain genetic markers may increase susceptibility to both conditions, explaining some of the overlap in their occurrence.
3.2 Neurobiological Factors
Both bipolar disorder and addiction involve dysregulation of the brain’s reward and pleasure centers. The neurotransmitter systems affected in bipolar disorder, particularly dopamine and serotonin, also play crucial roles in addiction processes.
3.3 Self-Medication Hypothesis
Many individuals with bipolar disorder turn to substances as a form of self-medication, attempting to alleviate symptoms or regulate mood swings. This can lead to a cycle of dependence and exacerbated mental health issues.
3.4 Environmental Stressors
Traumatic experiences, chronic stress, and unstable environments can contribute to the development of both bipolar disorder and substance use disorders.
4. Challenges in Diagnosis
Diagnosing co-occurring bipolar disorder and addiction presents unique challenges for mental health professionals.
4.1 Overlapping Symptoms
The symptoms of substance intoxication or withdrawal can mimic those of manic or depressive episodes, making it difficult to distinguish between the effects of substance use and genuine bipolar symptoms.
4.2 Temporal Relationship
Determining which condition developed first can be crucial for treatment planning but is often complicated by the intertwined nature of the symptoms.
4.3 Screening and Assessment Tools
Comprehensive screening tools and thorough clinical interviews are essential for accurate diagnosis. These may include mood charting, substance use history, and family history assessments.


5. Treatment Approaches for Dual Diagnosis
Effective treatment for co-occurring bipolar disorder and addiction requires an integrated approach that addresses both conditions simultaneously.
5.1 Integrated Treatment Models
Integrated treatment programs combine mental health and addiction services, offering a cohesive approach to addressing both disorders. This may include:
- Coordinated care between mental health and addiction specialists
- Comprehensive assessment and individualized treatment planning
- Dual focus on mood stabilization and substance use reduction
5.2 Pharmacological Interventions
Medication management is crucial in treating bipolar disorder and may include:
- Mood stabilizers (e.g., lithium, valproic acid)
- Antipsychotics
- Antidepressants (used cautiously due to risk of triggering mania)
For addiction treatment, medications may include:
- Naltrexone or acamprosate for alcohol dependence
- Buprenorphine or methadone for opioid addiction
5.3 Psychotherapeutic Approaches
Evidence-based psychotherapies play a vital role in treatment:
- Cognitive Behavioral Therapy (CBT): Helps identify and modify negative thought patterns and behaviors associated with both disorders.
- Dialectical Behavior Therapy (DBT): Focuses on emotional regulation and distress tolerance skills.
- Interpersonal and Social Rhythm Therapy (IPSRT): Addresses the disruption of biological and social rhythms in bipolar disorder.
- Motivational Enhancement Therapy: Helps individuals resolve ambivalence about substance use and treatment engagement.
5.4 Lifestyle Modifications
Encouraging healthy lifestyle changes can support recovery:
- Establishing regular sleep patterns
- Engaging in regular physical exercise
- Practicing stress-reduction techniques like mindfulness meditation
- Building a strong support network
6. Challenges in Recovery
Individuals with co-occurring bipolar disorder and addiction face unique challenges in their recovery journey:
6.1 Medication Compliance
Maintaining consistent medication adherence can be difficult, especially during manic episodes or when substance use interferes with treatment.
6.2 Relapse Prevention
The cyclical nature of bipolar disorder can complicate relapse prevention efforts for substance use. Mood episodes may trigger cravings or impulsive behavior leading to substance use.
6.3 Social and Occupational Functioning
Both conditions can significantly impact relationships, employment, and overall quality of life, requiring comprehensive support and rehabilitation efforts.
7. Future Directions in Research and Treatment
As our understanding of the relationship between bipolar disorder and addiction evolves, several areas of focus emerge for future research and treatment development:
7.1 Personalized Medicine Approaches
Advancing genetic and neuroimaging studies may lead to more personalized treatment plans based on individual biological markers and risk factors.
7.2 Novel Pharmacological Interventions
Research into new medications that can address both mood stabilization and addiction simultaneously is ongoing, with promising leads in glutamatergic and cholinergic systems.
7.3 Technology-Assisted Interventions
The development of mobile health applications and wearable devices for mood monitoring and early intervention shows potential in improving outcomes for individuals with dual diagnosis.
The Impact of Substance Use on Bipolar Disorder Patients
Bipolar disorder patients often struggle with the profound impact of co-occurring disorder like substance use. For these individuals, bipolar disorder symptoms can be further exacerbated by alcohol addiction or drug abuse, complicating their ability to maintain emotional regulation.
Alcohol use disorder, in particular, poses additional challenges as it can have depressant effects that interfere with mood stabilization. This makes recovery even more difficult for bipolar patients attempting to manage their condition.


Mixed Episodes and Co-occurring Substance Use
In bipolar patients, mixed episodes—a combination of manic and depressive symptoms—can make substance abuse issues more likely. The unpredictability of affective episodes leads some individuals to turn to illicit drugs for temporary relief, inadvertently creating a vicious cycle of substance dependency.
Mixed episodes also increase the likelihood of experiencing psychotic symptoms. Dual diagnosis treatment centers become essential for providing integrated care to manage both disorders effectively.
Common Risk Factors and Dual Diagnosis Challenges
The lifetime prevalence of comorbid substance use among individuals with bipolar disorder is notably high. Factors for addiction, such as high-risk, high-reward activities and intense emotions, often align with hypomanic symptoms.
This shared vulnerability makes the occurrence of comorbid substance dependency frequent. Furthermore, studies indicate that psychiatric comorbidity between bipolar disorder and substance use complicates diagnosis and treatment, demanding a nuanced understanding of the interplay between mental health disorder and substance abuse.
Affective Episodes and Secondary Substance Dependency
Affective symptoms, such as those seen in bipolar II or cyclothymic disorder, can increase the risk of secondary substance dependency. Episodes of depression or manic periods often encourage individuals to self-medicate with alcohol or other substances, which might initially seem to offer pleasurable effects or provide relief from distress.
However, drug addiction and alcohol abuse typically worsen the bipolar disorder experience. This necessitates ongoing substance abuse treatment to effectively manage the dual conditions.
Treatment Approaches for Dual Diagnosis
Bipolar disorder and addiction treatment requires specific approaches that consider both disorders simultaneously. Pharmacological treatment, including mood stabilizers, must be balanced to minimize bipolar disorder medication side effects, such as weight gain.
Integrated treatment for bipolar patients also focuses on psychotherapeutic interventions like Dialectical Behavior Therapy (DBT). This helps develop emotional regulation and distress tolerance skills.


Therapeutic Interventions for Long-term Recovery
Therapeutic interventions for dual diagnosis, such as individual therapy or weekly group therapy sessions, provide support for maintaining long-term recovery. Therapeutic modalities like Motivational Interviewing are effective for substance abuse treatment, helping bipolar disorder patients find reasons to avoid alcohol and drug use.
Additionally, family therapy plays a critical role in addressing relationship issues that arise from coexisting addiction and bipolar disorder. This holistic approach is key to maintaining recovery.
Mental Health Dual Diagnosis and Social Functioning
Mental disorders, such as bipolar and co-occurring substance use disorders, significantly impact daily life. Social skills often deteriorate due to intense mood swings and psychomotor agitation.
Integrated aftercare programmes and dual diagnosis support groups can help in restoring these essential social skills. They offer recovery resources and continued peer support.
Factors for Addiction and Anxiety Disorders
High prevalence rates of anxiety disorders and major depression are observed in bipolar patients. This contributes to the complexities of bipolar addiction comorbidity.
The presence of co-occurring anxiety often worsens substance-induced mood disorder, particularly during a manic period. Medical professionals and treatment strategies should include techniques for managing anxiety disorders alongside substance use.
Addressing Personality Disorders and Affective Symptoms
Comorbid substance dependency can also coincide with personality disorder in some cases. The National Institute of Mental Health suggests that untreated personality disorders further complicate the effectiveness of bipolar disorder and addiction treatment.
Addressing these underlying mental illnesses through dual disorders in bipolar individuals can enhance recovery outcomes. Effective therapies are needed for controlling affective symptoms, which frequently lead to damaging effects on both social relationships and daily functioning.
Impact of Behavioural Addictions on Bipolar Disorder
Behavioural addictions, such as internet addiction or gambling, are increasingly recognized as co-occurring issues in bipolar disorder. These addictions, often overlapping with affective episodes, contribute to the deterioration of activity levels and overall well-being.
The detrimental effects of behavioural addictions are similar to those observed in drug use disorders, complicating the course of treatment for bipolar disorder patients. Integrated treatment options must therefore include methods to address these behavioral addictions alongside substance use.
Innovative Treatment Strategies and Dual Diagnosis Management
Recent advancements in dual diagnosis management, such as the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD), offer promising results for individuals with co-occurring addictions. Effective dual diagnosis treatment centers aim to provide comprehensive and personalized approaches that address the unique challenges of substance abuse and bipolar disorder.
Pharmacological and psychotherapeutic approaches combined offer holistic support, reducing the odds ratio of relapse and supporting long-term, stable recovery. This integrated strategy is essential for sustained outcomes.


Co-occurring Disorders and Major Depression
Individuals experiencing co-occurring disorders often deal with both bipolar disorder and major depression. The relationship between bipolar disorder and major depression highlights the need for comprehensive treatment options that address depressive disorders alongside bipolar symptoms.
These individuals may also face additional challenges, such as personality disorders or anxiety, which can complicate their treatment journey. Tailored treatment plans that address these issues are necessary for recovery.
Daily Life and Emotional Regulation
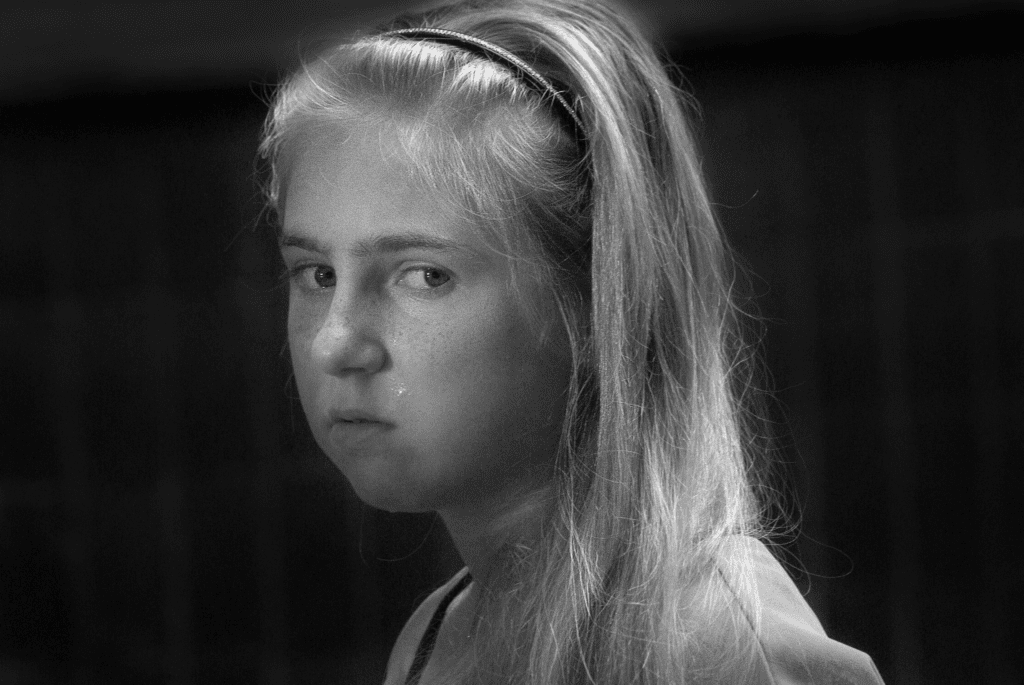
Bipolar disorder, also known as manic depression, significantly impacts an individual’s daily life. From mood swings to intense emotions, the ability to regulate these symptoms can be a constant battle.
Emotional regulation is key to managing bipolar disorder symptoms, particularly in the context of co-occurring substance abuse. Treatment programs are designed to help individuals establish healthier daily routines that aid in symptom management.
Suicidal Ideations and Comorbid Addictions
Suicidal ideations are a serious concern for bipolar disorder patients, particularly those who also suffer from comorbid addictions. Addiction can intensify depressive episodes and lead to an increase in suicidal thoughts.
Treatment options must incorporate interventions for addressing both suicidal ideations and substance abuse issues to ensure comprehensive care. This holistic approach helps mitigate risks and fosters stable recovery.
Bipolar Disorder Intervention Strategies
Intervention strategies for bipolar disorder often involve both pharmacological and psychotherapeutic methods. However, when co-occurring substance use is involved, more tailored approaches are necessary.
Integrated treatment for bipolar disorder and addiction helps manage manic periods, depressive episodes, and secondary substance dependency effectively. Customized intervention strategies ensure that the needs of each patient are met.
Secondary Substance Dependency and Recovery Support
Secondary substance dependency occurs when bipolar disorder patients develop a reliance on substances as a way of coping with their symptoms. Programs designed for addiction recovery for bipolar patients focus on managing both disorders simultaneously.
Aftercare programmes and support groups offer continued assistance for maintaining recovery from episodes of substance abuse and mood disorders. This support is vital for long-term success.
Bipolar Disorder Substance Abuse Statistics and Prevalence Rates
Bipolar disorder and addiction statistics reveal a high prevalence of substance abuse in individuals diagnosed with bipolar disorder. Studies have shown that the lifetime prevalence of substance use issues in bipolar patients is significantly greater compared to the general population.
Understanding these statistics is critical for shaping effective treatment approaches for individuals with co-occurring disorders. Early intervention and support can make a significant difference in outcomes.
Comorbid Substance Use and Behavioral Addictions
The occurrence of behavioral addictions, such as internet addiction, can further complicate the lives of bipolar disorder patients. Behavioral addictions have been linked to similar neurological pathways involved in drug use disorders.
Addressing these comorbid addictions is crucial for a successful recovery outcome. Treatment plans should include measures to tackle both substance use and behavioral addictions simultaneously.
Depressive Disorders and Mixed Episodes
Depressive disorders and mixed episodes are often seen in bipolar disorder patients struggling with substance use. Mixed episodes involve both manic and depressive features, leading to a heightened risk of substance abuse.
Treatment strategies need to address both the bipolar diagnosis and substance use to reduce the negative effects of mixed episodes. An integrated approach provides the best chance of recovery.
Psychomotor Agitation in Bipolar Disorder
Psychomotor agitation is a common symptom seen in both manic and depressive episodes of bipolar disorder. It may drive individuals towards substance use as a means to alleviate discomfort.
Addressing psychomotor agitation through individual therapy and pharmacological intervention is a crucial aspect of comprehensive treatment for bipolar disorder and addiction. Proper support can significantly alleviate these symptoms.
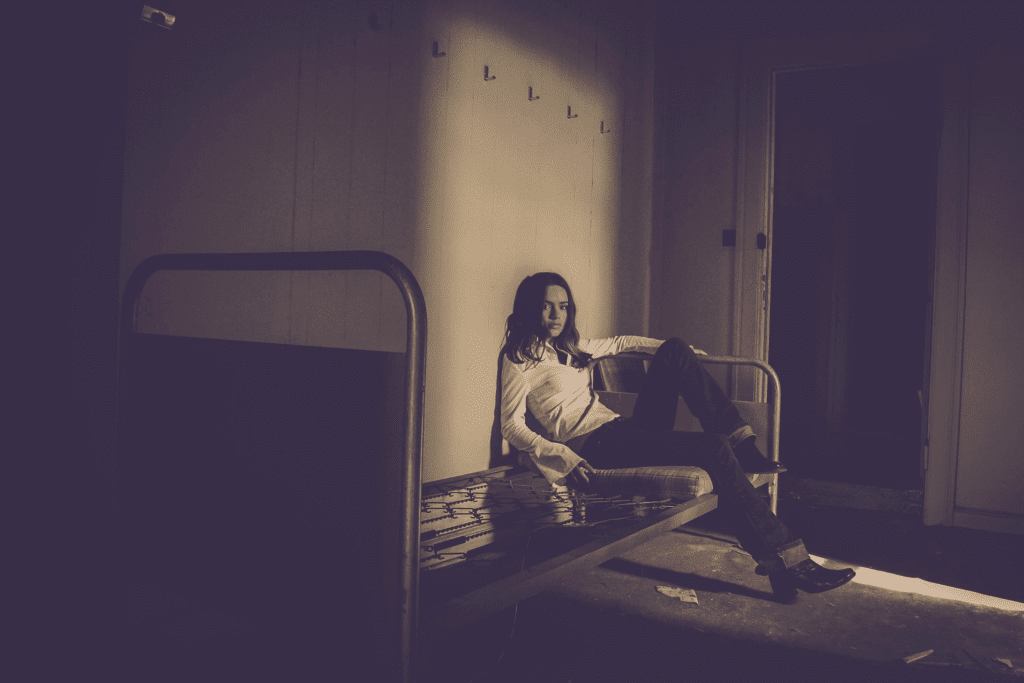
Real Life Impacts of Dual Diagnosis
The real life impact of dual diagnosis can be profound, affecting relationships, employment, and overall quality of life. Bipolar disorder and addiction therapy programs are designed to support patients in rebuilding their lives, fostering social skills, and ensuring that they have the tools needed to navigate daily challenges.
Integrated care involving medical professionals, support groups, and family dynamics is essential for recovery. These measures help patients achieve a stable and balanced lifestyle.
Coping Strategies and Treatment Resources
Coping strategies are essential for managing bipolar disorder and addiction. Resources such as dual diagnosis support groups, motivational interviewing, and assertiveness training help individuals develop the skills required for long-term stability.
Rehabilitation centers for bipolar disorder and addiction provide a structured environment for individuals to learn and practice these strategies. This support enhances the chances of successful outcomes.


Addressing Stigma and Myths Surrounding Bipolar Disorder and Addiction
Stigma and misconceptions surrounding bipolar disorder and addiction can be a major barrier to seeking help. Addressing these myths through education and awareness programs is crucial in ensuring individuals receive timely and appropriate treatment.
Bipolar disorder and addiction support groups also provide a sense of community, reducing isolation and encouraging individuals to engage in their recovery journey. Community support is a key element of long-term success.
StepRecovering from Addiction with Co-occurring Bipolar Disorder
Recovering from addiction may be particularly challenging for those with co-occurring bipolar disorder. Individuals often experience a substance-induced mood disorder, which exacerbates bipolar disorder symptoms.
Medical professionals must be well-versed in recognizing and managing these co-occurring issues to ensure effective treatment. Proper diagnosis and tailored intervention make a significant difference.
Integrated Treatment for Bipolar Disorder and Addiction
Integrated treatment models are highly recommended for those struggling with dual disorders in bipolar individuals. This type of treatment simultaneously addresses substance abuse treatment and bipolar disorder management, ensuring a cohesive approach to recovery.
Weekly group therapy sessions are part of the treatment, offering peer support and a sense of community. Peer engagement fosters resilience and accountability.
Addressing Long-Term Recovery for Bipolar Patients
Addiction recovery for bipolar patients requires careful planning and long-term management. It is crucial to maintain an individualized treatment plan to manage both conditions.
Long-term recovery is supported by aftercare programmes, ensuring patients continue to receive necessary support after completing a rehab for bipolar disorder and addiction. Ongoing care is vital for preventing relapse.
Weight Gain as a Side Effect of Bipolar Disorder Medication
Pharmacological treatment of bipolar disorder often involves mood stabilizers and antipsychotics, which may have side effects such as weight gain. The potential for weight gain can deter patients from remaining compliant with their medication.
Medical professionals must provide strategies to mitigate these effects while ensuring that bipolar disorder patients adhere to their prescribed regimen. This may include nutritional guidance and regular exercise.
Bipolar Diagnosis and Secondary Substance Dependency
A bipolar diagnosis often comes with the risk of secondary substance dependency, particularly among those with unmanaged symptoms. The desire for temporary relief from affective symptoms can lead to substance use, which further complicates bipolar disorder management.
Effective therapies, such as Cognitive Behavioral Therapy (CBT), can help address these tendencies by providing coping mechanisms for bipolar disorder and addiction. Structured support makes a significant difference.


Prevalence of Comorbid Addictions in Bipolar Disorder
The prevalence of comorbid addictions, such as alcohol addiction and drug abuse, is significantly higher in bipolar disorder patients compared to the general population. Factors for addiction in bipolar individuals include high activity levels during manic episodes and the tendency to engage in high-risk behaviors.
Medical professionals must account for these common risk factors when designing treatment plans for individuals with bipolar disorder. Comprehensive assessment is crucial for tailoring effective strategies.
Relationship Issues and Social Dynamics
Bipolar disorder, combined with substance use, often leads to relationship issues that affect family dynamics. Family therapy is an effective therapeutic approach that addresses these challenges.
Therapy provides strategies for family members to improve communication, understand the challenges of co-occurring disorders, and support their loved ones through recovery. Strong family involvement helps sustain long-term recovery.
Substance Abuse Treatment and Medical Professional Involvement
Substance abuse treatment for those with bipolar disorder must be handled by a medical professional experienced in dual diagnosis. Bipolar disorder and addiction require an integrated approach involving pharmacological treatment and psychotherapeutic interventions.
Medical professionals are crucial in ensuring that bipolar disorder and addiction treatment approaches are aligned for optimal recovery. Coordinated care is key to achieving stability.
Addressing Affective Symptoms in Bipolar Addiction Comorbidity
Affective symptoms such as intense emotions and mixed episodes are commonly observed in bipolar disorder patients with substance abuse issues. Managing these symptoms involves a combination of pharmacological and psychotherapeutic interventions.
Individual therapy and DBT are often utilized to provide patients with the skills needed for emotional regulation. Customized support helps address the specific needs of each individual.
Major Depression and Depressive Disorders in Bipolar Patients
Major depression and depressive disorders are commonly seen in individuals with bipolar disorder. These depressive phases can drive individuals towards substance use as a means of coping with a depressed mood.
Treatment strategies for bipolar disorder must focus on both affective and substance abuse symptoms to be effective. A balanced approach is necessary for successful management.
Addiction Recovery Resources for Bipolar Disorder Patients
Bipolar disorder patients require specialized addiction recovery resources that cater to their unique needs. Dual diagnosis treatment centers and integrated care models provide a combination of addiction and mental health services, offering a holistic approach to treatment.
These resources are crucial for bipolar disorder patients to achieve stable, long-term recovery from addiction. Ongoing support and structured care are key to achieving stability.
Comorbidity in Alcohol Use and Bipolar Disorder
Comorbidity in alcohol use and bipolar disorder is prevalent and often complicates the treatment process. Alcohol abuse can exacerbate depressive symptoms and hinder recovery from bipolar depression.
Addressing both the alcohol addiction and bipolar disorder in a coordinated treatment plan is essential for successful outcomes. Effective interventions are needed for managing these interlinked conditions.
Addressing Schizoaffective Disorders and Bipolar Disorder
Schizoaffective disorders can co-occur with bipolar disorder, adding complexity to the diagnosis and treatment. The presence of psychotic symptoms requires targeted interventions alongside traditional bipolar disorder treatment options.
Medical professionals need to recognize and address these overlapping symptoms to provide effective care. A tailored approach ensures the best outcomes for patients.
Illicit Drugs and Substance Use in Bipolar Disorder
The use of illicit drugs is common among bipolar disorder patients, as they often seek temporary relief from manic or depressive symptoms. Substance use can worsen the overall prognosis of bipolar disorder and lead to a cycle of dependency.
Addressing drug addiction through an integrated treatment model is crucial for managing both bipolar symptoms and substance abuse. This approach helps break the cycle of dependency.
Bipolar Disorder and the Role of Aftercare Programmes
Aftercare programmes play a vital role in supporting bipolar disorder patients post-rehabilitation. These programmes provide continued support, help prevent addiction relapse, and focus on maintaining mood stability.
Structured aftercare is essential for bipolar disorder patients to ensure long-term recovery and prevent recurrence of affective episodes. Consistent support is a key component of success.
Conclusion
The complex interplay between bipolar disorder and addiction presents significant challenges for individuals, families, and healthcare providers. However, with advances in integrated treatment approaches, pharmacological interventions, and psychotherapeutic techniques, there is hope for improved outcomes and quality of life for those affected by this dual diagnosis.
Understanding the intricate relationship between these conditions is crucial for developing effective prevention strategies, accurate diagnostic methods, and comprehensive treatment plans. As research continues to unravel the biological, psychological, and social factors underlying this comorbidity, we move closer to more targeted and efficacious interventions.
The journey towards recovery from co-occurring bipolar disorder and addiction is undoubtedly challenging, but with proper support, evidence-based treatment, and ongoing management, individuals can achieve stability, sobriety, and improved overall well-being. Continued efforts in research, clinical practice, and public awareness are essential in addressing this significant public health concern and providing hope for those affected by this dual diagnosis.
From Embrace Inner Chaos to your inbox
Transform your Chaos into authentic personal growth – sign up for our free weekly newsletter! Stay informed on the latest research advancements covering:
Narcissistic Personality Disorder (NPD)
Frequently Asked Questions
What Is The Relationship Between Bipolar Disorder And Addiction?
Bipolar disorder often co-occurs with substance abuse issues, creating a complex relationship between the two. The intense mood swings and emotional dysregulation associated with bipolar disorder may drive individuals to use substances like alcohol or drugs to find temporary relief.
This is especially true during manic periods, when high-risk, high-reward activities may seem more enticing. The National Institute on Drug Abuse emphasizes that people with mood disorders like bipolar are more prone to drug addiction due to the attempt to self-medicate or manage their mood symptoms.
Why Do Individuals With Bipolar Disorder Often Struggle With Alcohol Abuse?
Individuals with bipolar disorder often use alcohol to cope with their intense emotions, and the depressant effects of alcohol can seem to alleviate manic symptoms temporarily. However, alcohol use disorder often exacerbates symptoms of bipolar disorder, creating a vicious cycle.
According to American Addiction Centers, alcohol abuse may also trigger mixed episodes in bipolar disorder patients, where depressive and manic symptoms occur simultaneously, worsening the overall course of the mental health disorder.
How Do Bipolar Disorder Symptoms Impact Substance Use?
Bipolar disorder symptoms, including hypomanic symptoms and episodes of depression, have a profound impact on substance use patterns. During manic episodes, increased energy and impaired judgment may lead to risky behavior, including drug abuse.
Conversely, depressive episodes often lead to substance use as a form of escape or numbing of pain. The National Institute of Mental Health states that self-medication with substances can worsen both bipolar symptoms and substance dependency, making treatment for co-occurring disorders challenging.
What Are Common Risk Factors For Dual Diagnosis Of Bipolar Disorder And Addiction?
Common risk factors for dual diagnosis include family history of mood disorders, high stress levels, and a personal history of trauma or abuse. Factors like these often make individuals more vulnerable to both bipolar disorder and substance abuse issues, resulting in a co-occurring disorder.
Mental Health Services Administration identifies childhood trauma and psychiatric comorbidity as significant contributors to dual diagnosis, complicating the path to effective treatment and long-term recovery.
How Do Co-Occurring Disorders Affect Daily Life?
Co-occurring disorders, such as bipolar disorder and addiction, profoundly affect daily life, including maintaining employment, relationships, and general wellbeing. Individuals with both conditions often experience greater emotional regulation difficulties and struggle with adhering to treatment plans.
According to Dual Diagnosis Treatment Centers, these challenges can lead to frequent relapses and significant disruptions in daily routines, which necessitate a specialized treatment approach to achieve stability.
How Does Cyclothymic Disorder Relate To Substance Use?
Cyclothymic disorder, a milder form of bipolar disorder, also has a connection to substance abuse. Individuals with cyclothymic disorder may turn to alcohol or drugs as a way to cope with ongoing mood instability.
Calabrese J.R. reports that the fluctuating highs and lows of cyclothymic disorder can drive individuals towards substances to find some semblance of mood stability, thus increasing the lifetime prevalence of substance use among these individuals.
What Treatment Options Are Available For Co-Occurring Bipolar Disorder And Addiction?
There are several treatment options for co-occurring bipolar disorder and addiction, including pharmacological treatment, behavioral therapies like Dialectical Behaviour Therapy (DBT), and individual therapy. Integrated treatment programs are essential as they address both disorders simultaneously, improving outcomes for patients.
American Addiction Centers explain that medications like mood stabilizers are often used in tandem with therapies to help bipolar patients regain emotional control while addressing substance abuse issues.
How Do Mixed Episodes Complicate Addiction Treatment?
Mixed episodes, where symptoms of depression and mania occur simultaneously, greatly complicate addiction treatment. Patients may exhibit high levels of irritability, increased activity, and feelings of hopelessness at the same time, which makes stabilizing their mood challenging.
According to the National Institute on Drug Abuse, these complex symptoms often lead to inconsistent treatment adherence and increased substance use, as individuals struggle to manage their fluctuating symptoms.
What Is The Lifetime Prevalence Of Addiction Among Bipolar Patients?
The lifetime prevalence of addiction among bipolar patients is notably high, with some studies estimating that up to 60% of individuals with bipolar disorder also struggle with substance use disorder. The National Institute on Mental Health reports that this high rate of comorbidity complicates both diagnosis and treatment.
The presence of substance use disorder may mask or worsen the symptoms of bipolar disorder, making it more difficult to achieve stabilization.
How Can Emotional Regulation Help In Managing Bipolar Disorder And Addiction?
Emotional regulation is key in managing both bipolar disorder and addiction. Techniques such as mindfulness, cognitive behavioral strategies, and DBT help individuals process intense emotions without turning to substance use.
Dialectical Behaviour Therapy is particularly effective as it teaches distress tolerance skills, which allow individuals to better manage manic or depressive episodes without resorting to substance use, thereby breaking the cycle of dependency.
How Do Manic Periods Affect Substance Use?
Manic periods are characterized by increased activity levels, impulsivity, and diminished judgment, all of which increase the likelihood of substance use. Individuals experiencing mania may turn to drugs or alcohol as a means of heightening their euphoric state.
Systematic Treatment Enhancement Program for Bipolar Disorder emphasizes that substance use during manic episodes not only prolongs mania but also increases the severity of subsequent depressive episodes, which makes recovery more difficult.
How Does Alcohol Use Disorder Exacerbate Bipolar Disorder Symptoms?
Alcohol use disorder exacerbates bipolar disorder symptoms by intensifying mood swings, interfering with prescribed medications, and worsening episodes of depression. Alcohol’s depressant effects may deepen depressive symptoms, while its interference with medications can lead to uncontrolled manic or hypomanic symptoms.
The American Addiction Centers highlight that alcohol addiction is particularly detrimental to individuals with bipolar disorder, as it creates a barrier to effective treatment and recovery.
What Is The Role Of Individual Therapy In Dual Diagnosis Treatment?
Individual therapy plays a crucial role in treating dual diagnoses of bipolar disorder and addiction by addressing underlying emotional and psychological issues. Therapeutic techniques such as Motivational Interviewing help patients overcome ambivalence about quitting substance use while also managing their bipolar symptoms.
National Institute on Drug Abuse emphasizes that individual therapy tailored to address both disorders concurrently is effective in achieving long-term stability.
How Does Substance Abuse Treatment Differ For Bipolar Disorder Patients?
Substance abuse treatment for bipolar disorder patients involves a combination of psychiatric care, medications, and specialized therapy to manage both the mood disorder and addiction. Unlike standard substance abuse treatment, which may focus solely on detoxification, treatment for bipolar patients must also address mood stabilization and the prevention of manic or depressive episodes.
American Addiction Centers recommend integrated treatment programs that address all facets of the disorder, including medication management and emotional regulation strategies.


What Are The Detrimental Effects Of Drug Use On Bipolar Disorder?
Drug use can have numerous detrimental effects on individuals with bipolar disorder, including an increased frequency of mood episodes, heightened severity of symptoms, and greater resistance to medications. Mental Health Services Administration reports that drug use not only worsens the natural course of bipolar disorder but can also lead to more severe outcomes, such as psychotic symptoms and suicidal ideations.
This makes comprehensive treatment all the more crucial.
How Can Family Therapy Aid In Treating Bipolar Disorder And Addiction?
Family therapy addresses family dynamics that contribute to bipolar disorder and addiction, providing strategies for family members to better support their loved one. Understanding the disorder and the challenges of addiction helps families avoid enabling behaviors and fosters a supportive environment.
National Institute of Mental Health highlights that family involvement in therapy can greatly improve treatment adherence and outcomes by enhancing communication and reducing conflict.
What Challenges Arise In Treating Bipolar Addiction?
Challenges in treating bipolar addiction include the difficulty of managing mood instability, the risk of relapse, and resistance to treatment. The mood fluctuations of bipolar disorder often make it challenging for individuals to adhere to a treatment plan consistently.
According to Dual Diagnosis Treatment Centers, this dual struggle requires a well-coordinated, integrated treatment approach that includes medication, therapy, and support services to effectively manage both conditions.
How Do Mood Stabilizers Impact Substance Abuse In Bipolar Disorder?
Mood stabilizers are commonly used to help bipolar disorder patients manage mood swings, which in turn reduces their risk of substance abuse. These medications can prevent the high-risk behaviors associated with manic periods and help alleviate the depressive symptoms that often lead to self-medication.
American Addiction Centers note that when combined with behavioral therapies, mood stabilizers significantly reduce the chances of substance relapse in bipolar patients.
What Are Effective Strategies For Preventing Relapse In Bipolar Addiction?
Effective strategies for preventing relapse in bipolar addiction include maintaining a structured daily routine, engaging in weekly group therapy sessions, and taking prescribed medications regularly. Individual therapy and motivational interviewing can help bipolar patients stay focused on their recovery goals while addressing any underlying issues that could trigger relapse.
National Institute on Drug Abuse stresses that aftercare programs and support groups are also vital in helping patients navigate the challenges of daily life while maintaining sobriety.
How Do Mixed Episodes Affect Social Skills And Relationships In Bipolar Patients?
Mixed episodes, where individuals experience symptoms of both mania and depression, can severely affect social skills and interpersonal relationships. Individuals may act impulsively, be irritable, or withdraw from social interactions entirely, causing strain in relationships.
According to the American Addiction Centers, these fluctuating moods can make it challenging to maintain consistent behavior, leading to misunderstandings and conflict with friends and family members, ultimately affecting their support system.




