Last updated on December 18th, 2024 at 06:36 am
- 1.1 Defining Recurrent Depression
- 1.2 The Impact of Recurrent Depression
- 2. Risk Factors for Recurrent Depressive Episodes
- 2.1 Genetic Predisposition
- 2.2 Early Life Experiences
- 2.3 Chronic Stress and Life Events
- 2.4 Personality Traits and Cognitive Patterns
- 2.5 Comorbid Mental Health Conditions
- 3. Recognizing the Signs of a Depressive Episode
- 3.1 Emotional Symptoms
- 3.2 Cognitive Symptoms
- 3.3 Physical Symptoms
- 3.4 Behavioral Changes
- 4. Treatment Approaches for Recurrent Depression
- 4.1 Psychotherapy
- 4.2 Medication
- 4.3 Combination Therapy
- 4.4 Lifestyle Modifications
- 4.5 Alternative and Complementary Therapies
- 5. Strategies for Preventing Recurrent Depressive Episodes
- 5.1 Developing a Relapse Prevention Plan
- 5.2 Building a Strong Support Network
- 5.3 Practicing Mindfulness and Self-Awareness
- 5.4 Maintaining Consistent Treatment
- 6. The Role of Research and Future Directions
- 6.1 Neurobiological Factors
- 6.2 Novel Treatment Modalities
- 6.3 Digital Mental Health Interventions
- 6.4 Precision Medicine Approaches
- 7. Neurobiological Factors in Recurrent Depression
- 8. Depression and HPA Axis Dysregulation
- 9. Chronic Pain and Depression
- 10. Depression and Neuroplasticity
- 11. Depression and Medical Illnesses
- 12. Environmental Triggers and Stressful Life Events
- 13. Depression and Sleep Disturbances
- 14. Depression and Personality Traits
- 15. Depression and Brain Stimulation Therapies
- 16. Depression and Gut-Brain Interaction
- 17. Genetic Factors and Depression
- 18. Depression and Hormonal Imbalances
- 19. Depression and Comorbid Psychopathology
- 20. Depression and Cognitive Behavioral Therapy (CBT)
- 21. Depression and Lifestyle Factors
- 22. Clinical Trials and Emerging Treatments
- 23. Depression and Mitochondrial Dysfunction
- 24. Depression and Inflammation
- 25. Depression and Oxidative Stress
- 26. Depression and Epigenetics
- 27. Depression and Neurotransmitter Imbalance
- 28. Depression and Long-Term Treatment
- 29. Depression and Major Depression
- 30. Depression and Seasonal Affective Disorder
- 31. Depression and Social Isolation
- 32. Depression and Coping Mechanisms
- 33. Depression and Chronic Depression Causes
- 34. Depression and Clinical Depression
- 35. Depression and Unipolar Depression
- 36. Depression and Dysphoric Disorder
- 37. Depression and Mood Stabilizers
- 38. Depression and Psychiatric Disorders
- 39. Depression and Traumatic Events
- 40. Depression in Primary Care Settings
- 41. Depression and Functional Impairment
- 42. Depression and Previous Episode
- 43. Depression and Residual Symptoms
- 44. Depression and Onset of Depression
- 45. Depression and Psychotic Symptoms
- Frequently Asked Questions
- What Are The Key Risk Factors For Recurrent Depressive Episodes?
- How Does Bipolar Disorder Contribute To The Risk Of Depression Relapse?
- Is There A Link Between Stressful Life Events And Recurrent Depression?
- How Does Treatment-Resistant Depression Increase The Risk Of Recurrence?
- Can Magnetic Stimulation Reduce The Risk Of Recurrent Depressive Episodes?
- How Do Hormonal Imbalances Affect The Recurrence Of Depression?
- What Is The Role Of Childhood Trauma In Recurrent Depression?
- Can Chronic Medical Illnesses Increase The Risk Of Depression Relapse?
- How Does Genetic Predisposition Influence The Recurrence Of Depression?
- How Do Residual Symptoms Contribute To The Recurrence Of Depression?
- Can Lifestyle Factors Influence The Likelihood Of Recurrent Depression?
- Does The Severity Of Depression Impact The Risk Of Recurrence?
- How Do Antidepressant Medications Impact The Risk Of Depression Recurrence?
- What Role Does Sleep Disturbance Play In Recurrence Of Depressive Episodes?
- How Does Social Isolation Contribute To The Recurrence Of Depression?
- Can Cognitive Behavioral Therapy (CBT) Prevent Recurrence Of Depression?
- How Do Traumatic Events Influence The Likelihood Of Recurrent Depression?
- What Role Do Mood Stabilizers Play In Preventing Recurrent Depressive Episodes?
- Can Antidepressant Therapies Fail To Prevent Recurrence Of Depression?
- How Does The Presence Of Comorbid Psychiatric Disorders Impact Recurrence Of Depression?
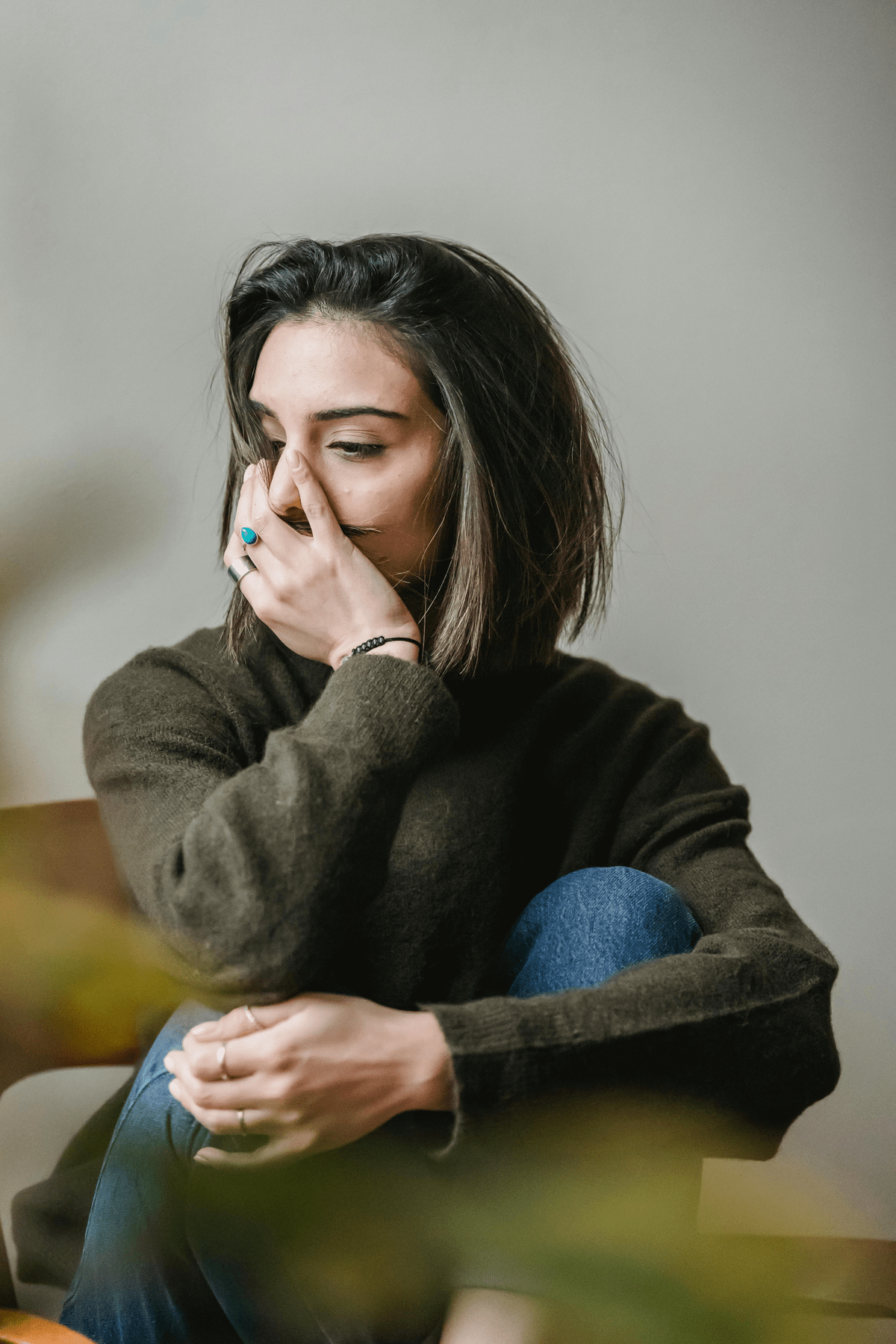
Depression is a complex mental health condition that affects millions of people worldwide. While many individuals experience occasional bouts of sadness or low mood, recurrent depressive episodes can significantly impact a person’s quality of life and overall well-being.
These episodes are characterized by persistent feelings of hopelessness, loss of interest in daily activities, and a range of physical and emotional symptoms that can last for weeks or even months.
1.1 Defining Recurrent Depression
Recurrent depression refers to the repeated occurrence of major depressive episodes over time. Unlike single-episode depression, which may resolve with treatment and not return, recurrent depression involves multiple episodes throughout a person’s lifetime. These episodes can vary in frequency, severity, and duration, making it a challenging condition to manage.
1.2 The Impact of Recurrent Depression
The effects of recurrent depression extend far beyond emotional distress. Individuals experiencing repeated depressive episodes may struggle with:
- Impaired work performance and reduced productivity
- Strained relationships with family and friends
- Difficulty maintaining a consistent self-care routine
- Increased risk of substance abuse or other unhealthy coping mechanisms
- Higher likelihood of developing chronic health conditions
Understanding the nature of recurrent depression is crucial for developing effective treatment strategies and support systems for those affected by this condition.
2. Risk Factors for Recurrent Depressive Episodes
Several factors can contribute to an increased likelihood of experiencing recurrent depressive episodes. By identifying these risk factors, healthcare professionals and individuals can work together to develop targeted prevention and treatment approaches.
2.1 Genetic Predisposition
Research has shown that genetics play a significant role in the development of recurrent depression. Individuals with a family history of depression, particularly among first-degree relatives, are at a higher risk of experiencing multiple depressive episodes throughout their lives. While having a genetic predisposition does not guarantee the development of depression, it can increase susceptibility to environmental triggers and stressors.


2.2 Early Life Experiences
Childhood trauma, neglect, or adverse experiences can significantly impact an individual’s mental health in adulthood. These early life events may alter brain structure and function, making a person more vulnerable to recurrent depressive episodes. Examples of influential early life experiences include:
- Physical, emotional, or sexual abuse
- Loss of a parent or primary caregiver
- Chronic illness or disability
- Exposure to domestic violence or substance abuse
- Severe bullying or social isolation
2.3 Chronic Stress and Life Events
Prolonged exposure to stress can significantly increase the risk of recurrent depressive episodes. Major life events, both positive and negative, can trigger depressive symptoms in vulnerable individuals. Some common stressors include:
- Job loss or financial instability
- Divorce or relationship breakdowns
- Death of a loved one
- Chronic illness or injury
- Significant life transitions (e.g., moving, starting a new job)
2.4 Personality Traits and Cognitive Patterns
Certain personality traits and cognitive patterns may predispose individuals to recurrent depression. These include:
- Neuroticism: A tendency to experience negative emotions more intensely
- Perfectionism: Setting unrealistically high standards for oneself
- Negative self-talk and rumination
- Low self-esteem and poor self-image
- Difficulty with emotional regulation
2.5 Comorbid Mental Health Conditions
The presence of other mental health disorders can increase the likelihood of experiencing recurrent depressive episodes. Common comorbid conditions include:
- Anxiety disorders
- Bipolar disorder
- Post-traumatic stress disorder (PTSD)
- Substance use disorders
- Eating disorders
3. Recognizing the Signs of a Depressive Episode
Early identification of depressive symptoms is crucial for timely intervention and prevention of recurrent episodes. While the manifestation of depression can vary from person to person, there are several common signs to watch for:
3.1 Emotional Symptoms
- Persistent feelings of sadness, emptiness, or hopelessness
- Irritability or mood swings
- Loss of interest in previously enjoyed activities
- Feelings of worthlessness or excessive guilt
- Difficulty experiencing pleasure or joy
3.2 Cognitive Symptoms
- Impaired concentration and decision-making abilities
- Memory problems
- Negative thought patterns and self-talk
- Suicidal thoughts or ideation
- Difficulty planning for the future
3.3 Physical Symptoms
- Changes in sleep patterns (insomnia or excessive sleeping)
- Appetite changes and fluctuations in weight
- Fatigue and low energy levels
- Unexplained aches and pains
- Slowed speech or movements
3.4 Behavioral Changes
- Social withdrawal and isolation
- Neglect of personal hygiene and self-care
- Decreased productivity at work or school
- Increased use of alcohol or other substances
- Engaging in risky or self-destructive behaviors


4. Treatment Approaches for Recurrent Depression
Managing recurrent depression often requires a comprehensive, multi-faceted approach. While there is no one-size-fits-all solution, several evidence-based treatments have shown effectiveness in reducing the frequency and severity of depressive episodes.
4.1 Psychotherapy
Various forms of psychotherapy can be beneficial for individuals with recurrent depression:
- Cognitive Behavioral Therapy (CBT): Helps identify and change negative thought patterns and behaviors
- Interpersonal Therapy (IPT): Focuses on improving relationships and communication skills
- Mindfulness-Based Cognitive Therapy (MBCT): Combines mindfulness techniques with cognitive therapy to prevent relapse
- Psychodynamic Therapy: Explores unconscious thoughts and past experiences that may contribute to depression
4.2 Medication
Antidepressant medications can be an important component of treatment for recurrent depression. Common types include:
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
- Atypical antidepressants
- Tricyclic antidepressants
- Monoamine Oxidase Inhibitors (MAOIs)
It’s important to work closely with a healthcare provider to find the most effective medication and dosage, as individual responses can vary.
4.3 Combination Therapy
For many individuals with recurrent depression, a combination of psychotherapy and medication proves most effective. This approach addresses both the psychological and biological aspects of depression, potentially leading to better outcomes and reduced risk of relapse.
4.4 Lifestyle Modifications
Implementing healthy lifestyle changes can significantly impact the course of recurrent depression:
- Regular exercise and physical activity
- Maintaining a balanced, nutritious diet
- Prioritizing sleep hygiene and establishing consistent sleep patterns
- Stress management techniques (e.g., meditation, deep breathing exercises)
- Limiting alcohol consumption and avoiding recreational drugs
4.5 Alternative and Complementary Therapies
Some individuals may find benefit in exploring alternative or complementary therapies alongside traditional treatments:
- Acupuncture
- Herbal supplements (e.g., St. John’s Wort, under medical supervision)
- Light therapy for seasonal affective disorder
- Art or music therapy
- Yoga or tai chi
5. Strategies for Preventing Recurrent Depressive Episodes
While it may not be possible to completely prevent recurrent depressive episodes, several strategies can help reduce their frequency and severity:
5.1 Developing a Relapse Prevention Plan
Working with a mental health professional to create a personalized relapse prevention plan can be invaluable. This plan typically includes:
- Identifying early warning signs of depression
- Listing coping strategies and support resources
- Outlining steps to take when symptoms emerge
- Specifying when to seek professional help
5.2 Building a Strong Support Network
Maintaining strong social connections can provide crucial emotional support during difficult times. This may involve:
- Nurturing relationships with family and friends
- Joining support groups for individuals with depression
- Engaging in community activities or volunteering
- Considering peer support programs
5.3 Practicing Mindfulness and Self-Awareness
Developing mindfulness skills can help individuals become more aware of their thoughts and emotions, allowing for earlier intervention when depressive symptoms arise. Techniques may include:
- Daily meditation or mindfulness exercises
- Keeping a mood journal
- Practicing gratitude
- Engaging in regular self-reflection
5.4 Maintaining Consistent Treatment
For individuals with a history of recurrent depression, maintaining consistent treatment even during periods of remission can be crucial. This may involve:
- Regular check-ins with a mental health professional
- Adhering to prescribed medication regimens
- Continuing therapy or counseling sessions
- Participating in maintenance treatment programs


6. The Role of Research and Future Directions
Ongoing research in the field of recurrent depression continues to shed light on its underlying mechanisms and potential treatment approaches. Some promising areas of study include:
6.1 Neurobiological Factors
Advances in neuroimaging and genetic research are providing new insights into the biological basis of recurrent depression. This knowledge may lead to more targeted and personalized treatment approaches in the future.
6.2 Novel Treatment Modalities
Emerging therapies such as transcranial magnetic stimulation (TMS), ketamine infusions, and psychedelic-assisted psychotherapy are showing promise for treatment-resistant depression and may offer new options for individuals with recurrent depressive episodes.
6.3 Digital Mental Health Interventions
The development of smartphone apps, online therapy platforms, and other digital tools is expanding access to mental health resources and support for individuals with recurrent depression.
6.4 Precision Medicine Approaches
Researchers are working towards developing more personalized treatment plans based on an individual’s genetic, biological, and environmental factors, potentially improving outcomes for those with recurrent depression.
7. Neurobiological Factors in Recurrent Depression
Neurobiological mechanisms play a key role in the risk of relapse. Dysfunctions in brain chemistry, such as serotonin deficiency and dopamine dysfunction, are often implicated in recurrent episodes of depression.
This neurochemical imbalance contributes to both the severity of depression and its persistence over time. Addressing these imbalances is key to mitigating recurrent depressive episodes.
8. Depression and HPA Axis Dysregulation
Dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis has been linked to depressive disorder. Elevated cortisol levels can exacerbate a depressed mood, particularly in individuals experiencing severe depression or a severe episode.
This physiological response can lead to further episodes of depression, thereby increasing the risk of recurrence. Effective regulation of the HPA axis may be crucial for long-term management.
9. Chronic Pain and Depression
Chronic pain is a major risk factor for recurrent depressive episodes. People with depression are often found to have comorbid chronic pain, which further complicates the treatment of depression.
The interaction between pain and depression symptoms can prolong episode duration and contribute to a chronic condition. Managing pain effectively is critical in reducing depressive symptoms.
10. Depression and Neuroplasticity
Recent research has highlighted the role of neuroplasticity in depression. Recurrent episodes of depression can reduce neurogenesis, particularly in the hippocampus, which is crucial for emotional regulation.
Depression and hippocampal atrophy are associated with increased functional impairment and diminished response to antidepressant treatment. Promoting neuroplasticity can improve treatment outcomes.
11. Depression and Medical Illnesses
Medical conditions like cardiovascular disease and diabetes significantly increase the risk of recurrent depressive episodes. Depression and cardiovascular disease often coexist, resulting in worse outcomes for both.
Similarly, depression in patients with diabetes can hinder effective disease management, contributing to chronic depression. Addressing these medical conditions holistically can alleviate depression symptoms.
12. Environmental Triggers and Stressful Life Events
Stressful life events such as divorce, job loss, or financial instability can contribute to the onset of depression and elevate the risk of recurrence. Psychological stress and depression are closely linked, with environmental triggers of depression often catalyzing a subsequent episode.
This highlights the importance of managing stress as a preventive strategy. Coping mechanisms and social support can be instrumental in mitigating these triggers.


13. Depression and Sleep Disturbances
Sleep disturbances are common in people with depression and often play a significant role in depression recurrence prevention. Poor sleep quality can worsen depressive symptoms, making a person more vulnerable to another episode of depression.
Effective management of sleep disturbances is often a component of successful treatment for depression. Sleep hygiene and medication can help improve sleep patterns.
14. Depression and Personality Traits
Certain personality traits, such as neuroticism and perfectionism, are associated with a higher risk of relapse. Depression and personality traits such as low emotional resilience or poor coping mechanisms can contribute to the chronic nature of the mood disorder.
These traits also contribute to the severity of depression symptoms in each episode. Developing resilience and adaptive coping skills can mitigate the risk of relapse.
15. Depression and Brain Stimulation Therapies
Brain stimulation therapies, such as electroconvulsive therapy and transcranial magnetic stimulation, are options for treatment-resistant depression. These treatments are often considered when standard treatments fail, particularly for those experiencing severe symptoms or a severe episode.
Emerging techniques like magnetic stimulation show promise in reducing depressive symptoms in treatment-resistant cases Cleveland Clinic. Continued research into these therapies is crucial for expanding treatment options.


16. Depression and Gut-Brain Interaction
The gut microbiome is increasingly recognized for its role in depression. Depression and gut microbiome imbalances can lead to inflammation, which is thought to contribute to depressive disorder.
This connection between gut health and mental health suggests potential treatment approaches, such as probiotics, for alleviating symptoms of depression American Journal of Psychiatry. Integrating diet and probiotics may enhance standard depression treatments.
17. Genetic Factors and Depression
Genetic predisposition to depression is a major risk factor for recurrent episodes. The presence of genetic factors like a family history of depression can predispose individuals to forms of depression that are chronic and recurring.
This genetic susceptibility is often triggered by environmental stressors, leading to an episode of depression Journal of Affective Disorders. Identifying these genetic markers can help develop personalized treatment plans.
18. Depression and Hormonal Imbalances
Hormonal imbalances, particularly related to the reproductive cycle, can contribute to the development of depression. Postpartum depression risk factors include hormonal shifts that occur after childbirth.
Similarly, hormonal imbalances and depression during menopause can lead to increased rates of depression among women Health Organization. Timely hormonal interventions can mitigate these risks.
19. Depression and Comorbid Psychopathology
The presence of other psychiatric disorders significantly increases the risk of recurrence. Anxiety comorbidity with depression, for example, can complicate both the treatment of depression and the management of other mental health conditions.
Depression and bipolar disorder, in particular, pose unique challenges in primary care settings due to their overlapping symptoms and treatment needs American Psychiatric Association. Coordinated care is essential for managing these complexities.


20. Depression and Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy for depression is a commonly used approach in both initial treatment and long-term management. CBT helps individuals reframe negative thought patterns that contribute to depressive episodes.
It is particularly effective in reducing the risk of recurrence by equipping individuals with better coping skills Acta Psychiatrica Scandinavica. Consistent CBT practice can prevent future episodes.
21. Depression and Lifestyle Factors
Lifestyle factors affecting depression include physical inactivity, poor diet, and social isolation. Depression and obesity, for instance, are linked, with each condition exacerbating the other.
Incorporating physical activity and maintaining a balanced diet can mitigate depressive symptoms and reduce the likelihood of a subsequent episode. Addressing lifestyle factors is key in the long-term treatment for depression.
22. Clinical Trials and Emerging Treatments
Clinical trials are crucial in evaluating new treatments for recurrent depression. Novel therapies, including psychedelic-assisted psychotherapy and ketamine infusions, show promise for severe, treatment-resistant depression.
These approaches offer hope for those who do not respond to usual care or antidepressant therapies, providing alternative options for individuals with chronic depression American College of Physicians. Participation in clinical trials can expand access to cutting-edge treatments.
23. Depression and Mitochondrial Dysfunction
Mitochondrial dysfunction has been linked to recurrent episodes of depression. Studies suggest that abnormalities in mitochondrial energy production can contribute to depressive disorder.
This dysfunction may explain the chronic fatigue often experienced by people with depression and its role in subsequent episode development. Targeting mitochondrial health may improve treatment outcomes.


24. Depression and Inflammation
Inflammation is a critical factor in the development and recurrence of depression. Chronic inflammation can lead to neuroinflammation, which contributes to depression symptoms.
Understanding the relationship between depression and inflammation helps in the development of anti-inflammatory treatment strategies to reduce the risk of relapse. Dietary and pharmacological interventions may play a role.
25. Depression and Oxidative Stress
Oxidative stress is another physiological mechanism implicated in depression. High levels of oxidative stress can damage neural tissue, contributing to the severity of depression.
Addressing oxidative stress through antioxidants or lifestyle interventions can be part of a successful treatment for depression, particularly in treatment-resistant cases. Reducing oxidative damage may help in lowering the recurrence rate.
26. Depression and Epigenetics
Epigenetics provides insights into how environmental triggers of depression can alter gene expression without changing the underlying DNA. Depression and gene-environment interaction explain why individuals with genetic predisposition may or may not develop depression based on their life experiences.
These findings have significant implications for personalized antidepressant therapies. Adjusting treatment approaches based on epigenetic markers may yield better results.
27. Depression and Neurotransmitter Imbalance
Norepinephrine and depression are closely linked due to their role in mood regulation. A neurotransmitter imbalance involving norepinephrine, serotonin, and dopamine can lead to severe depression symptoms.
Antidepressant medication efficacy often hinges on targeting these neurotransmitters to restore balance and reduce depressive symptoms. Personalized treatment focusing on neurotransmitter regulation can be effective.


28. Depression and Long-Term Treatment
Long-term treatment approaches are crucial for people with chronic or recurrent depression. Maintaining ongoing antidepressant treatment and regular psychotherapy sessions can prevent the progression from mild depression to a severe episode.
Long-term treatment strategies can reduce the risk of recurrence and improve overall outcomes American Psychiatric Association 2013. Adherence to these strategies can enhance quality of life.
29. Depression and Major Depression
Major depression can significantly impact an individual’s quality of life and contribute to a chronic condition if left untreated. It is one of the most severe forms of depression, often necessitating comprehensive treatment involving antidepressant therapies and lifestyle changes.
Timely intervention is crucial to prevent the progression to major depressive disorder. Addressing symptoms early can lead to a better prognosis.
30. Depression and Seasonal Affective Disorder
Seasonal affective disorder risk factors include reduced exposure to natural sunlight during winter months. This type of depression can be addressed through light therapy, which is effective in mitigating the symptoms of depression associated with seasonal changes.
This preventive measure can help reduce the onset of seasonal depressive episodes. Monitoring light exposure and supplementing with vitamin D can also be beneficial.
31. Depression and Social Isolation
Social isolation and depression are mutually reinforcing, making it critical to address isolation as part of depression management. Depression in adults, particularly older adults, is often linked to a lack of social support, which can prolong episode duration and increase the risk of recurrence.
Strengthening social ties is a preventive measure against recurrent episodes. Community engagement and support groups can be effective in reducing isolation.


32. Depression and Coping Mechanisms
Effective coping mechanisms can significantly reduce the risk of recurrence in people with depression. Poor coping strategies are linked to a higher risk of relapse, whereas cognitive behavioral approaches and resilience training have been found effective in mitigating symptoms of depression.
Fostering healthy coping skills is integral to depression recurrence prevention. Mindfulness and stress reduction techniques are also useful tools.
33. Depression and Chronic Depression Causes
Chronic depression causes include a combination of genetic predisposition, environmental stressors, and comorbid medical illnesses. Depression and diabetes, for example, often interact to create a cycle of poor health outcomes, thereby increasing the risk of a chronic depressive disorder.
Comprehensive treatment approaches are needed to address these intertwined factors. Lifestyle changes, combined with medical management, can improve outcomes for chronic depression.
34. Depression and Clinical Depression
Clinical depression, characterized by a persistently depressed mood and functional impairment, often requires a combination of antidepressant medication and psychotherapy. It is crucial to recognize and treat clinical depression early to avoid chronicity.
Timely intervention can prevent the progression from a clinical episode to a more severe form of depression. Early diagnosis and adherence to treatment plans can improve quality of life.
35. Depression and Unipolar Depression
Unipolar depression is a type of depression without manic episodes, distinguishing it from bipolar disorder. Individuals with unipolar depression often experience more frequent recurrences if untreated.
Effective treatment for depression, particularly in its early stages, can prevent unipolar depression from becoming a long-term issue. Regular follow-ups can help maintain stability.
36. Depression and Dysphoric Disorder
Dysphoric disorder involves intense depressive episodes characterized by severe symptoms, including irritability and mood swings. It is a severe episode of depression that requires immediate treatment.
Recognizing dysphoric disorder early helps in providing appropriate interventions and preventing a subsequent episode. Treatment often involves medication and supportive therapies.


37. Depression and Mood Stabilizers
Mood stabilizers are often used alongside antidepressants in the treatment of mood disorders, especially when comorbid with bipolar disorder. These medications help prevent severe mood fluctuations and contribute to the successful treatment of depressive symptoms.
The use of mood stabilizers can reduce the likelihood of a relapse. Long-term monitoring and adjustment of medication are key to effective management.
38. Depression and Psychiatric Disorders
Psychiatric disorders like disruptive mood dysregulation disorder and major depressive disorder often coexist with recurrent depressive episodes. The presence of multiple forms of psychopathology increases the complexity of treatment.
Early intervention in psychiatric disorders can significantly impact the duration of symptoms and improve treatment outcomes. Integrated care models can help address these coexisting issues.
39. Depression and Traumatic Events
A traumatic event is often a trigger for the onset of depression or a recurrent depressive episode. Depression and childhood trauma are strongly linked, with early adverse experiences increasing vulnerability to depression later in life.
Trauma-informed care is essential for effectively addressing the needs of people with depression stemming from past trauma. Therapy that focuses on healing trauma can improve long-term outcomes.
40. Depression in Primary Care Settings
Managing depression in primary care is often the first step for individuals seeking help. Primary care settings play a vital role in the diagnosis and initial treatment of depression, particularly for mild depression.
Collaborative care models, involving mental health services and primary care, enhance outcomes in the treatment for depression. These models ensure continuity of care and comprehensive management.
41. Depression and Functional Impairment
Functional impairment due to depression can significantly reduce quality of life. Depression in adolescents, for instance, often manifests as impaired school performance and social withdrawal, necessitating timely intervention.
Effective treatment aims to restore functioning and reduce impairment in individuals with depressive disorder. Addressing functional goals is crucial for long-term success.


42. Depression and Previous Episode
A previous episode of depression increases the risk of future episodes. The risk of relapse is particularly high if the previous episode was untreated or inadequately managed.
Long-term strategies focusing on maintenance therapy can help prevent recurrent episodes. Ongoing support and adherence to treatment are key preventive measures.
43. Depression and Residual Symptoms
Residual symptoms are common even after successful treatment of an acute episode of depression. These symptoms can increase the likelihood of a subsequent episode if not properly addressed.
Continuous monitoring and intervention are crucial to mitigate residual symptoms and reduce the risk of recurrence. Follow-up care is essential for lasting remission.
44. Depression and Onset of Depression
The onset of depression can occur at any age, with particular risk factors varying across the lifespan. Depression in children, for instance, may be triggered by social isolation or bullying, whereas depression in older adults may relate to chronic illnesses.
Early intervention during the onset of depression can prevent long-term consequences. Screening and early therapy are important for mitigating future risks.
45. Depression and Psychotic Symptoms
Severe depression can sometimes be accompanied by psychotic symptoms, such as delusions or hallucinations. This form of depression requires specialized care, often involving a combination of antidepressant and antipsychotic medications.
Recognizing and treating psychotic symptoms early can prevent the worsening of depressive episodes. Integrated treatment approaches are necessary for managing complex cases.
From Embrace Inner Chaos to your inbox
Transform your Chaos into authentic personal growth – sign up for our free weekly newsletter! Stay informed on the latest research advancements covering:
Narcissistic Personality Disorder (NPD)
Frequently Asked Questions
What Are The Key Risk Factors For Recurrent Depressive Episodes?
Key risk factors for recurrent depressive episodes include a combination of genetic, biological, and environmental influences. People with a family history of depression have a higher likelihood of experiencing recurrent episodes due to a genetic predisposition.
Moreover, chronic stressors, such as ongoing financial or interpersonal issues, can increase vulnerability to future episodes. Hormonal imbalances, especially involving the hypothalamic-pituitary-adrenal (HPA) axis, have also been shown to play a critical role in increasing the likelihood of recurrence according to Cleveland Clinic.
How Does Bipolar Disorder Contribute To The Risk Of Depression Relapse?
Bipolar disorder, characterized by alternating mood episodes of depression and mania, significantly increases the risk of depression relapse. During periods of remission, individuals may still experience residual symptoms, which elevate the chances of relapse.
Unipolar depression, often part of bipolar disorder’s depressive episodes, is also more challenging to treat due to mood instability. Moreover, according to the American Psychiatric Association, the shifting nature of bipolar disorder requires ongoing treatment and monitoring, as symptoms may return without proper management.
Is There A Link Between Stressful Life Events And Recurrent Depression?
Stressful life events, such as losing a loved one, job stress, or going through a divorce, are known triggers for recurrent episodes of depression. These events may activate the underlying biological pathways of depression, involving changes in the HPA axis and heightened cortisol levels, making individuals more susceptible to future episodes.
Studies reported in the American Journal of Psychiatry indicate that people who experience multiple stressful life events have a higher risk of recurrence, especially when no stress-coping strategies are employed.
How Does Treatment-Resistant Depression Increase The Risk Of Recurrence?
Treatment-resistant depression, which refers to a condition that does not respond adequately to standard antidepressant therapies, often leads to recurrent depressive episodes. Individuals with treatment-resistant depression frequently face extended bouts of depression, which leads to a higher cumulative risk of relapse.
As per findings shared by the Cleveland Clinic, without a successful response to initial treatment, patients remain vulnerable, and many require alternative treatments, such as electroconvulsive therapy or brain stimulation therapies, to manage symptoms effectively.


Can Magnetic Stimulation Reduce The Risk Of Recurrent Depressive Episodes?
Magnetic stimulation, particularly repetitive transcranial magnetic stimulation (rTMS), is increasingly used for patients with treatment-resistant depression. This non-invasive treatment aims to stimulate brain regions associated with mood regulation, notably the prefrontal cortex, to alleviate symptoms.
According to a study published by Cleveland Clinic, rTMS has shown promise in reducing the recurrence rate for patients by enhancing neuroplasticity, thereby enabling individuals to better manage depressive symptoms and resist relapse.
How Do Hormonal Imbalances Affect The Recurrence Of Depression?
Hormonal imbalances, particularly in the regulation of cortisol through the HPA axis, can heighten the risk of recurrent depressive episodes. Elevated cortisol levels, often triggered by chronic stress or medical conditions, can adversely affect brain regions such as the hippocampus, leading to increased vulnerability to depression.
The American Psychiatric Association points out that individuals with consistent hormonal fluctuations have a higher tendency for recurrence if the underlying imbalance is not addressed properly.
What Is The Role Of Childhood Trauma In Recurrent Depression?
Childhood trauma is a significant risk factor for the development of recurrent depressive episodes later in life. Traumatic experiences during formative years can lead to alterations in brain chemistry and structure, such as increased sensitivity to stress and dysregulation of neurotransmitters.
Research cited by Acta Psychiatrica Scandinavica suggests that individuals exposed to early trauma often face heightened vulnerability to depressive episodes, as unresolved trauma tends to re-emerge during stressful situations.
Can Chronic Medical Illnesses Increase The Risk Of Depression Relapse?
Chronic medical illnesses, such as cardiovascular disease, diabetes, or chronic pain, can significantly raise the risk of recurrent depressive episodes. These medical conditions often lead to physical and emotional stress, further exacerbating depressive symptoms and affecting mood regulation.
As noted by the American College of Physicians, the added burden of managing a chronic illness, alongside the direct physiological effects, can increase the probability of depression relapsing in patients with previous depressive disorders.
How Does Genetic Predisposition Influence The Recurrence Of Depression?
A genetic predisposition to depression plays a critical role in the likelihood of recurrent episodes, particularly in individuals with a family history of mood disorders. Genetic factors affect neurotransmitter regulation, brain structure, and susceptibility to environmental stressors.
According to a Journal of Affective Disorders article, individuals with first-degree relatives who have experienced major depressive disorder or bipolar disorder are at a significantly increased risk of facing recurrent episodes themselves.


How Do Residual Symptoms Contribute To The Recurrence Of Depression?
Residual symptoms, which are those depressive symptoms that linger even after a major depressive episode subsides, are a strong predictor of recurrence. These symptoms, which may include fatigue, low mood, and sleep disturbances, make it difficult for patients to return to full psychosocial functioning, thereby increasing the likelihood of future episodes.
According to Fava M, patients with residual symptoms often require targeted intervention beyond standard antidepressant therapies to avoid relapses.
Can Lifestyle Factors Influence The Likelihood Of Recurrent Depression?
Lifestyle factors such as physical inactivity, unhealthy eating habits, and lack of sleep can play a significant role in the recurrence of depression. Regular physical exercise has been shown to positively impact brain chemistry and promote neuroplasticity, thereby lowering the risk of recurrent episodes.
As per findings from the Cleveland Clinic, individuals who fail to engage in these protective lifestyle behaviors are at higher risk for depression relapse due to a lack of support for healthy brain function and coping mechanisms.
Does The Severity Of Depression Impact The Risk Of Recurrence?
The severity of an initial depressive episode is directly correlated with the risk of recurrence. Individuals experiencing severe symptoms, such as psychotic symptoms or marked functional impairment, are more likely to experience subsequent depressive episodes.
According to the American Journal of Psychiatry, those with severe episodes are more challenging to treat effectively and often require long-term treatment strategies, including both pharmacological and therapeutic interventions, to prevent recurrence.
How Do Antidepressant Medications Impact The Risk Of Depression Recurrence?
Antidepressant medications, particularly selective serotonin reuptake inhibitors (SSRIs), are commonly used in preventing depression recurrence by stabilizing mood and addressing symptoms. However, discontinuation or non-compliance with medication increases the risk of relapse, especially in individuals with chronic depression.
The American Psychiatric Association emphasizes the importance of maintaining treatment adherence for an extended duration, even after symptom improvement, to effectively reduce the risk of recurrent depressive episodes.
What Role Does Sleep Disturbance Play In Recurrence Of Depressive Episodes?
Sleep disturbances, including insomnia and hypersomnia, are not only symptoms of depression but also predictors of future depressive episodes. Sleep dysregulation can impair cognitive functioning, affect stress responses, and ultimately contribute to the recurrence of depressive episodes.
According to Simon GE, addressing sleep issues early through therapeutic interventions can be critical in preventing the re-emergence of depressive symptoms in individuals with a history of mood disorders.
How Does Social Isolation Contribute To The Recurrence Of Depression?
Social isolation is a significant risk factor for depression recurrence, as the absence of a supportive social network can exacerbate feelings of loneliness, despair, and worthlessness. Social interactions are known to boost positive neurotransmitter activity and provide emotional support that can buffer against depressive symptoms.
According to Cuijpers P, individuals who are socially isolated or have poor social relationships are more likely to relapse compared to those with strong support systems.
Can Cognitive Behavioral Therapy (CBT) Prevent Recurrence Of Depression?
Cognitive Behavioral Therapy (CBT) is a highly effective non-pharmacological approach for reducing the risk of depression recurrence. CBT helps individuals recognize and alter maladaptive thinking patterns and behaviors that contribute to depression, thus equipping them with tools to manage symptoms proactively.
According to the Cleveland Clinic, CBT has been shown to significantly reduce the rates of relapse by providing patients with coping mechanisms that help them deal with stress and negative thought patterns.
How Do Traumatic Events Influence The Likelihood Of Recurrent Depression?
Traumatic events, such as physical or emotional abuse, can profoundly increase the likelihood of recurrent depression by altering stress response mechanisms in the brain. Trauma often leads to heightened HPA axis activity, leading to excessive cortisol release, which has been linked to mood disorders.
Research from Acta Psychiatrica Scandinavica shows that individuals with a history of trauma are at significantly higher risk for experiencing repeated episodes of depression, especially if left untreated.
What Role Do Mood Stabilizers Play In Preventing Recurrent Depressive Episodes?
Mood stabilizers, such as lithium, are often used to manage bipolar disorder and prevent depressive episodes from recurring. These medications work by reducing the fluctuations in mood that predispose individuals to depressive and manic episodes.
According to the American Psychiatric Association, consistent use of mood stabilizers can help maintain mood stability, thereby reducing the risk of depressive relapse, particularly for individuals with a history of severe mood instability.
Can Antidepressant Therapies Fail To Prevent Recurrence Of Depression?
Despite their effectiveness in initial treatments, antidepressant therapies sometimes fail to prevent the recurrence of depression due to incomplete symptom remission or inadequate treatment duration. Individuals who discontinue antidepressants prematurely are at an especially high risk of relapse.
The American Journal of Psychiatry notes that prolonged treatment, sometimes for several years, may be necessary to minimize the risk of recurrence, particularly for patients with recurrent or treatment-resistant forms of depression.
How Does The Presence Of Comorbid Psychiatric Disorders Impact Recurrence Of Depression?
The presence of comorbid psychiatric disorders, such as anxiety or substance abuse disorders, significantly increases the risk of recurrent depressive episodes. Comorbid conditions can complicate treatment, reduce the effectiveness of antidepressant therapies, and contribute to greater functional impairment.
According to research by Katon W, patients with both anxiety and depressive symptoms are particularly prone to experiencing recurrent episodes due to the heightened overall burden of mental health challenges and difficulties in achieving full remission.



