Last updated on December 18th, 2024 at 07:31 am
- 1. The Origins and Development of DMDD as a Diagnosis
- 1.1 Historical Context of Mood Disorders in Children
- 2. Core Symptoms and Diagnostic Criteria
- 2.1 Persistent Irritability and Anger
- 2.2 Severe Temper Outbursts
- 2.3 Chronicity and Age of Onset
- 2.4 Impairment in Multiple Settings
- 3. Differentiating DMDD from Other Disorders
- 3.1 DMDD vs. Bipolar Disorder
- 3.2 DMDD vs. Oppositional Defiant Disorder (ODD)
- 3.3 DMDD vs. Major Depressive Disorder (MDD)
- 4. Etiology and Risk Factors
- 4.1 Genetic Factors
- 4.2 Neurobiological Factors
- 4.3 Environmental and Psychosocial Factors
- 4.4 Temperamental Factors
- 5. Assessment and Diagnosis
- 5.1 Clinical Interview
- 5.2 Standardized Assessment Tools
- 5.3 Medical Evaluation
- 5.4 Observational Assessment
- 6. Treatment Approaches
- 6.1 Psychosocial Interventions
- 6.2 Pharmacological Treatment
- 6.3 School-Based Interventions
- 7. Long-Term Outcomes and Prognosis
- 7.1 Psychiatric Comorbidities
- 7.2 Functional Impairment
- 7.3 Risk for Adult Mood Disorders
- 8. Future Directions and Challenges
- 8.1 Refining Diagnostic Criteria
- 8.2 Developing Targeted Treatments
- 8.3 Understanding Developmental Trajectories
- 8.4 Addressing Cultural and Contextual Factors
- Neurobiological Factors and Brain Imaging Studies
- The Role of Genetic and Environmental Influences
- DMDD and Comorbid Conditions
- Assessing Irritability in Pediatric Patients
- DMDD and Social Relationships
- Parent Training for Managing DMDD
- DMDD in School Settings
- DMDD and Academic Performance
- Pharmacological Treatments for DMDD
- Technological Tools for Tracking DMDD Symptoms
- Cultural Considerations in DMDD Diagnosis
- DMDD and Sensory Processing Issues
- Mindfulness Techniques for Children with DMDD
- Role of Pediatricians in Diagnosing DMDD
- DMDD and Sleep Disturbances
- DMDD and Trauma History
- Family Therapy Approaches for DMDD
- DMDD and Executive Functioning Deficits
- Role of Diet and Nutrition in Managing DMDD
- Proposed Disruptive Mood Dysregulation Disorder
- Impact of DMDD on Sibling Relationships
- DMDD and Self-Esteem in Children
- DMDD and Adolescent Substance Use
- Differentiating DMDD from Bipolar Disorder Diagnoses
- DMDD and Autism Spectrum Disorder
- Conduct Disorder and DMDD
- DMDD and Sensory Processing Disorder
- Strategies for Reducing Temper Tantrums in Children
- Technological Advances in DMDD Treatment
- DMDD and Vitamin Deficiency
- DMDD and Non-Motor Symptoms
- Field Trials and Clinical Trials on DMDD
- Early Signs of Disruptive Mood Dysregulation Disorder
- DMDD and Risk of Developing Depression
- DMDD and Emotional Regulation Skills
- DMDD and Academic Accommodations
- DMDD and Functional Outcomes
- DMDD and Anger Management Techniques
- DMDD and Peer Interactions
- DMDD and Language Development
- DMDD and Suicide Ideation
- Parent Support Groups for Disruptive Mood Dysregulation Disorder
- Intramural Research Program on DMDD
- Conclusion
- Frequently Asked Questions
- What Are the Key Symptoms of Disruptive Mood Dysregulation Disorder?
- How Is Disruptive Mood Dysregulation Disorder Diagnosed?
- How Does DMDD Differ From Bipolar Disorder in Youth?
- What Are the Common Comorbidities Associated With DMDD?
- What Treatment Options Are Available for DMDD?
- How Effective Is Cognitive-Behavioral Therapy in Treating DMDD?
- Can DMDD Be Managed Without Medication?
- How Does DMDD Impact Family Dynamics?
- What Role Do Pediatricians Play in Diagnosing DMDD?
- How Does DMDD Affect Academic Performance?
- What Are the Long-Term Outcomes for Children Diagnosed With DMDD?
- How Is DMDD Related to Severe Mood Dysregulation?
- What Are the Differences Between DMDD and Oppositional Defiant Disorder (ODD)?
- How Do Parent Training Programs Help in Managing DMDD?
- Can DMDD Lead to Other Mental Health Issues in Adolescence?
- What Are Some Strategies for Reducing Temper Outbursts in Children With DMDD?
- How Does DMDD Affect Social Relationships in Children?
- How Do Neurobiological Factors Contribute to DMDD?
- Are There Cultural Considerations in the Diagnosis of DMDD?
- How Can School-Based Interventions Help Children With DMDD?
Disruptive Mood Dysregulation Disorder (DMDD) is a relatively new psychiatric diagnosis that has gained increasing attention in recent years. This condition primarily affects children and adolescents, characterized by persistent irritability, anger, and frequent, intense temper outbursts.
As a newly recognized disorder, DMDD presents unique challenges for mental health professionals, families, and affected individuals.
1. The Origins and Development of DMDD as a Diagnosis
DMDD was first introduced in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013. Its inclusion was motivated by concerns about the over-diagnosis of bipolar disorder in children and adolescents. Prior to DMDD’s recognition, many young people exhibiting chronic irritability and severe temper outbursts were often misdiagnosed with bipolar disorder, leading to potentially inappropriate treatment approaches.
The development of DMDD as a distinct diagnosis aimed to provide a more accurate framework for understanding and treating children with severe, persistent mood dysregulation that did not fit neatly into existing diagnostic categories. This shift in diagnostic approach has significant implications for treatment strategies and long-term outcomes for affected individuals.
1.1 Historical Context of Mood Disorders in Children
To fully appreciate the significance of DMDD’s inclusion in the DSM-5, it’s essential to understand the historical context of mood disorders in pediatric populations. For decades, clinicians struggled to accurately diagnose and treat children exhibiting severe mood dysregulation and behavioral problems. The lack of a specific diagnostic category for these symptoms often led to misdiagnosis or over-diagnosis of conditions like bipolar disorder or oppositional defiant disorder.
The recognition of DMDD represents a paradigm shift in how mental health professionals conceptualize and approach chronic irritability and anger in young people. This change reflects growing awareness of the unique developmental aspects of mood regulation in children and adolescents.
2. Core Symptoms and Diagnostic Criteria
DMDD is characterized by a constellation of symptoms that significantly impact a child’s daily functioning and quality of life. The primary features of DMDD include:
2.1 Persistent Irritability and Anger
Children with DMDD experience persistent irritability and anger that is present most of the day, nearly every day. This irritable or angry mood is observable by others, such as parents, teachers, or peers, and is out of proportion to the situation or provocation.
2.2 Severe Temper Outbursts
A hallmark of DMDD is the presence of severe, recurrent temper outbursts that are grossly out of proportion to the situation. These outbursts can be verbal (e.g., screaming, yelling) or behavioral (e.g., physical aggression towards people or property). The frequency and intensity of these outbursts exceed what would be typically expected for the child’s developmental level.
2.3 Chronicity and Age of Onset
For a diagnosis of DMDD, symptoms must be present for at least 12 months, with no symptom-free period lasting three months or longer. The onset of symptoms typically occurs before age 10, but the diagnosis is not given to children younger than 6 or older than 18 years.
2.4 Impairment in Multiple Settings
The symptoms of DMDD must cause significant impairment in at least two settings, such as at home, at school, or with peers. This criterion highlights the pervasive nature of the disorder and its impact on various aspects of the child’s life.


3. Differentiating DMDD from Other Disorders
One of the primary challenges in diagnosing DMDD is distinguishing it from other mood and behavioral disorders that share similar symptoms. Accurate differential diagnosis is crucial for determining appropriate treatment approaches.
3.1 DMDD vs. Bipolar Disorder
While DMDD and bipolar disorder can both involve irritability and mood dysregulation, there are key differences:
– Episodic nature: Bipolar disorder is characterized by distinct episodes of mania or hypomania alternating with periods of depression. In contrast, DMDD involves persistent irritability without clear-cut mood episodes.
– Age of onset: Bipolar disorder typically emerges in late adolescence or early adulthood, while DMDD symptoms often appear in childhood.
– Family history: Bipolar disorder has a stronger genetic component, with a higher likelihood of family history compared to DMDD.
3.2 DMDD vs. Oppositional Defiant Disorder (ODD)
DMDD and ODD share features of defiance and irritability, but differ in important ways:
– Severity of outbursts: DMDD involves more severe and frequent temper outbursts compared to ODD.
– Persistence of irritability: While children with ODD may experience irritability, it is typically not as pervasive or chronic as in DMDD.
– Intentionality: ODD often involves deliberate defiance and vindictiveness, whereas DMDD outbursts are more reactive and less intentional.
3.3 DMDD vs. Major Depressive Disorder (MDD)
Although both DMDD and MDD involve mood disturbances, they differ in presentation:
– Nature of mood symptoms: MDD is characterized by persistent sadness or loss of interest, while DMDD primarily involves irritability and anger.
– Cognitive symptoms: MDD often includes cognitive symptoms like difficulty concentrating or feelings of worthlessness, which are not central features of DMDD.
– Course of illness: MDD typically involves discrete episodes, while DMDD symptoms are more chronic and persistent.
4. Etiology and Risk Factors
The exact causes of DMDD are not fully understood, but research suggests a complex interplay of genetic, neurobiological, and environmental factors.
4.1 Genetic Factors
While specific genes associated with DMDD have not been identified, there is evidence of a genetic component to mood dysregulation and irritability. Children with first-degree relatives who have mood disorders may be at increased risk for developing DMDD.
4.2 Neurobiological Factors
Emerging research suggests that children with DMDD may have differences in brain structure and function, particularly in areas involved in emotion regulation and impulse control. Abnormalities in the amygdala, prefrontal cortex, and their connections have been implicated in the pathophysiology of DMDD.
4.3 Environmental and Psychosocial Factors
Various environmental factors may contribute to the development or exacerbation of DMDD symptoms:
– Chronic stress or trauma
– Inconsistent or harsh parenting practices
– Family conflict or instability
– Peer rejection or bullying
– Academic difficulties
4.4 Temperamental Factors
Certain temperamental traits, such as high emotional reactivity or low frustration tolerance, may increase a child’s vulnerability to developing DMDD.
5. Assessment and Diagnosis
Accurately diagnosing DMDD requires a comprehensive assessment that considers multiple sources of information and rules out other potential causes of the child’s symptoms.
5.1 Clinical Interview
A thorough clinical interview with the child and caregivers is essential for gathering information about symptom onset, duration, severity, and impact on functioning. The interview should explore the child’s developmental history, family history of mental health disorders, and any potential environmental stressors.
5.2 Standardized Assessment Tools
Various standardized assessment tools can aid in the diagnosis of DMDD:
– Child Behavior Checklist (CBCL)
– Mood and Feelings Questionnaire (MFQ)
– Affective Reactivity Index (ARI)
– Strengths and Difficulties Questionnaire (SDQ)
These measures can help quantify the severity of symptoms and track changes over time.
5.3 Medical Evaluation
A medical evaluation may be necessary to rule out potential physical causes of irritability or mood dysregulation, such as thyroid dysfunction or neurological conditions.
5.4 Observational Assessment
Direct observation of the child’s behavior in various settings (e.g., home, school) can provide valuable information about the nature and frequency of temper outbursts and irritability.
6. Treatment Approaches
Treatment for DMDD typically involves a multimodal approach that combines psychosocial interventions with pharmacological treatment when necessary.
6.1 Psychosocial Interventions
Evidence-based psychosocial treatments for DMDD include:
– Cognitive Behavioral Therapy (CBT): Helps children identify and modify negative thought patterns and develop coping skills for managing anger and irritability.
– Parent Management Training: Teaches parents strategies for effectively managing their child’s behavior and improving parent-child interactions.
– Dialectical Behavior Therapy (DBT): Focuses on enhancing emotion regulation skills and mindfulness techniques.
– Social Skills Training: Addresses difficulties in peer relationships and social functioning.
6.2 Pharmacological Treatment
While no medications are specifically FDA-approved for DMDD, several classes of medications may be used to target specific symptoms:
– Stimulants: May help with attention and impulse control if comorbid ADHD is present.
– Antidepressants: SSRIs may be beneficial for managing irritability and mood symptoms.
– Atypical antipsychotics: In severe cases, these medications may be considered for managing aggression and severe mood dysregulation.
– Mood stabilizers: Some children may benefit from mood stabilizers, although evidence is limited.
6.3 School-Based Interventions
Collaboration with school personnel is crucial for managing DMDD symptoms in the educational setting. Interventions may include:
– Individualized Education Plans (IEPs) or 504 plans
– Classroom accommodations to reduce triggers for outbursts
– Social-emotional learning programs
– Regular communication between parents and teachers


7. Long-Term Outcomes and Prognosis
As DMDD is a relatively new diagnosis, long-term outcome studies are limited. However, available research suggests that children with DMDD are at increased risk for various adverse outcomes in adolescence and adulthood.
7.1 Psychiatric Comorbidities
Children with DMDD have higher rates of comorbid psychiatric disorders, including anxiety disorders, depression, and substance use disorders. Early intervention and effective treatment may help mitigate these risks.
7.2 Functional Impairment
Persistent DMDD symptoms can lead to significant functional impairment in academic, social, and occupational domains. Addressing these challenges early on is crucial for improving long-term outcomes.
7.3 Risk for Adult Mood Disorders
Some studies suggest that children with DMDD may be at increased risk for developing major depressive disorder or anxiety disorders in adulthood. Ongoing research is needed to better understand the long-term trajectory of DMDD.
8. Future Directions and Challenges
As our understanding of DMDD continues to evolve, several key areas require further research and attention:
8.1 Refining Diagnostic Criteria
Ongoing research is needed to validate and potentially refine the diagnostic criteria for DMDD, particularly in differentiating it from other mood and behavioral disorders.
8.2 Developing Targeted Treatments
There is a need for more targeted, evidence-based treatments specifically designed for DMDD. This includes both psychosocial interventions and potential pharmacological approaches.
8.3 Understanding Developmental Trajectories
Longitudinal studies are crucial for elucidating the developmental course of DMDD and identifying factors that influence long-term outcomes.
8.4 Addressing Cultural and Contextual Factors
Further research is needed to understand how cultural and contextual factors may influence the presentation, diagnosis, and treatment of DMDD across diverse populations.


Neurobiological Factors and Brain Imaging Studies
Recent research has highlighted potential neurobiological underpinnings of disruptive mood dysregulation disorder. Studies using magnetic resonance imaging have revealed abnormalities in areas of the brain responsible for emotional regulation and impulse control, such as the prefrontal cortex and amygdala.
The National Institute of Mental Health has been at the forefront of investigating these structural and functional differences. These insights may help explain the severe mood dysregulation observed in children with DMDD.
The Role of Genetic and Environmental Influences
Both genetic and environmental factors play crucial roles in the development of disruptive mood dysregulation disorder. Children with first-degree relatives who have mood disorders are at a higher risk of developing DMDD.
Adverse childhood experiences, such as chronic family conflict or family divorce, significantly contribute to irritability in children. These environmental stressors increase the likelihood of DMDD symptoms and highlight the need for comprehensive family-focused interventions.


DMDD and Comorbid Conditions
DMDD frequently coexists with other mental health conditions, complicating the diagnostic process. Children with DMDD symptoms often present with attention-deficit/hyperactivity disorder or anxiety disorders.
Differentiating DMDD from oppositional defiant disorder and conduct disorder remains challenging due to overlapping behavioral symptoms, such as irritable behaviors and aggressive behavior. Accurate diagnosis is critical to avoid diagnostic error and ensure appropriate treatment.
Assessing Irritability in Pediatric Patients
Accurate assessment of irritability in pediatric patients requires a thorough understanding of symptom criteria. Clinicians often use standardized assessment tools and interviews to evaluate irritability-related impairment.
Identifying early signs of disruptive mood dysregulation disorder can facilitate timely interventions. These interventions can improve functional outcomes and reduce severe irritability.
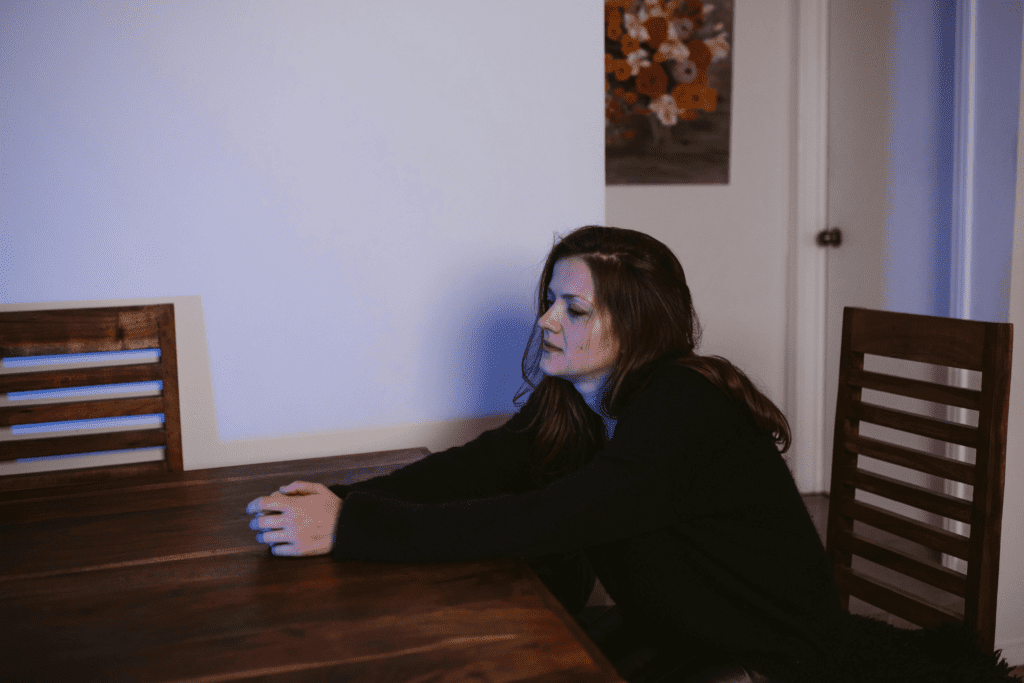
DMDD and Social Relationships
DMDD significantly impacts a child’s social relationships. The irritable-angry mood and temper outbursts characteristic of DMDD often lead to peer rejection.
Peer rejection can further contribute to social withdrawal and negative mood. Managing chronic irritability in youth through evidence-based interventions can improve peer interactions and foster better social relationships.
Parent Training for Managing DMDD
Parent training for managing DMDD is an essential component of treatment. Parents of children with DMDD symptoms often struggle with their child’s irritable mood and recurrent temper tantrums.
Parent management training programs are designed to equip parents with strategies to address explosive disorder-like behaviors. These strategies can reduce temper tantrums in children and improve overall family dynamics.
DMDD in School Settings
Identifying DMDD in school settings is critical for early intervention. Teachers can play an important role in recognizing disruptive behavior disorder symptoms, such as severe temper tantrums and verbal outbursts.
Collaboration between school staff and mental health professionals can result in effective school-based interventions for disruptive mood dysregulation disorder. These interventions include individualized education plans and social-emotional learning initiatives.
DMDD and Academic Performance
DMDD can have a profound impact on academic performance. Severe mood dysregulation often leads to difficulty focusing, poor school attendance, and impaired peer relationships.
Early intervention programs for mood dysregulation are crucial to help children overcome academic challenges. Involving both educators and mental health professionals can improve their overall educational experience.


Pharmacological Treatments for DMDD
Pharmacological treatments for mood dysregulation in youth are used when behavioral interventions alone are insufficient. Medications for disruptive mood dysregulation disorder may include stimulants for attention issues or SSRIs for managing irritable mood symptoms.
While pharmacological treatment can be helpful, it is most effective when combined with psychosocial interventions. Cognitive-behavioral therapy can complement medication to provide a comprehensive treatment approach.
Technological Tools for Tracking DMDD Symptoms
Technological tools are increasingly being used to track DMDD symptoms in real-time. Mobile applications and online platforms allow parents and clinicians to monitor the frequency of outburst symptoms and irritable behaviors.
This data can help inform treatment adjustments and support early intervention efforts. Such tools ultimately aim to reduce irritability in youth and improve functional outcomes.
Cultural Considerations in DMDD Diagnosis
Cultural considerations play a significant role in the diagnosis of DMDD. The presentation of symptoms, including irritability in youth and emotional dysregulation, may vary across different cultural backgrounds.
Clinicians must consider cultural norms and expectations regarding child behavior to avoid potential biases in the diagnostic process. Understanding cultural influences can lead to more accurate diagnoses and tailored treatment strategies.
DMDD and Sensory Processing Issues
Some children with DMDD also struggle with sensory processing issues, which can exacerbate irritable mood symptoms. These sensory challenges can lead to more frequent aggressive behavior.
Addressing sensory sensitivities through occupational therapy or sensory integration activities can be beneficial for these children. It helps them better manage their emotional responses and cope more effectively.
Mindfulness Techniques for Children with DMDD
Mindfulness techniques are emerging as effective strategies for reducing temper outbursts in children with DMDD. Practices such as guided meditation and breathing exercises can help children regulate their emotional responses.
Integrating mindfulness into therapy for children with DMDD may enhance emotional regulation skills. This can improve overall treatment outcomes and reduce the frequency of irritable-angry mood episodes.
Role of Pediatricians in Diagnosing DMDD
Pediatricians play a key role in the early identification of DMDD. Through regular assessments of behavioral symptoms, such as recurrent temper tantrums and severe irritability, pediatricians can identify children at risk.
Early referral to a specialist can lead to timely diagnosis. This reduces the risk of long-term emotional dysregulation and improves functional outcomes.
DMDD and Sleep Disturbances
Sleep disturbances are common in children with DMDD. These disturbances can often exacerbate emotional dysregulation and negative mood.
Addressing sleep hygiene as part of the treatment plan can help reduce irritability. Cognitive-behavioral approaches focusing on sleep are an effective adjunct to other therapies for managing chronic irritability.


DMDD and Trauma History
A history of trauma can increase a child’s vulnerability to developing DMDD. Exposure to adverse events, such as abuse or neglect, can contribute to severe temper outbursts in adolescents.
Trauma-informed care is essential when treating children with DMDD. Ensuring interventions are sensitive to the child’s past experiences helps foster resilience and emotional stability.
Family Therapy Approaches for DMDD
Family therapy approaches for DMDD involve the entire family in the treatment process. Engaging parents and siblings in therapy can help reduce irritability-related impairment.
Strategies such as communication training and problem-solving skills are often used to address defiant and aggressive behavior. These strategies promote a more harmonious family environment.
DMDD and Executive Functioning Deficits
Executive functioning deficits, such as difficulties with planning and impulse control, are often observed in children with DMDD. These deficits contribute to emotional dysregulation and outburst symptoms.
Addressing executive functioning through targeted interventions, such as cognitive-behavioral strategies, may help improve emotional regulation. This can ultimately reduce disruptive mood dysregulation disorder symptoms.
Role of Diet and Nutrition in Managing DMDD
The role of diet and nutrition in managing DMDD is an emerging area of interest. Nutritional deficiencies, such as vitamin deficiency, may contribute to irritability and mood dysregulation in children.
Ensuring a balanced diet rich in essential nutrients could help mitigate some of these emotional symptoms. This approach can complement other treatment modalities like therapy and medication.
Proposed Disruptive Mood Dysregulation Disorder
Proposed disruptive mood dysregulation disorder was initially conceptualized to address concerns about the over-diagnosis of bipolar disorder in children. This new classification aimed to differentiate chronic irritability and severe temper tantrums from manic episodes.
Experts like Ellen Leibenluft from the National Institute of Mental Health contributed significantly to the conceptualization of DMDD. This differentiation helps ensure more appropriate diagnoses and treatment plans for children.


Impact of DMDD on Sibling Relationships
The impact of DMDD on sibling relationships is often profound. Siblings may experience stress and confusion due to the irritable behaviors of the affected child.
Support strategies, including family therapy and sibling support groups, can help alleviate these stresses. Addressing the needs of siblings is vital for maintaining a stable family environment.
DMDD and Self-Esteem in Children
DMDD can significantly affect self-esteem in children. Recurrent temper tantrums and difficulty with peer relationships can lead to feelings of failure.
Implementing positive reinforcement techniques is crucial in fostering a healthy self-esteem in children with DMDD. Focusing on building resilience helps mitigate the impact of negative mood on self-worth.
DMDD and Adolescent Substance Use
Adolescents with DMDD are at an increased risk for substance use. Emotional dysregulation and frequent angry outbursts may lead some youths to use substances as a coping mechanism.
Early intervention and engagement in therapy are essential to address substance use risks. Cognitive-behavioral therapy can help promote healthier coping strategies.
Differentiating DMDD from Bipolar Disorder Diagnoses
Differentiating DMDD from bipolar disorder diagnoses is essential, as treatment approaches vary significantly. Unlike bipolar disorder, which involves episodic mood swings including hypomanic episodes, DMDD is characterized by persistent irritability.
Accurate differentiation helps in applying appropriate therapeutic approaches. This can reduce the risk of treatment-resistant symptoms and improve outcomes.
DMDD and Autism Spectrum Disorder
Children diagnosed with DMDD may also present symptoms overlapping with autism spectrum disorder. These may include social impairments and irritable mood.
Differentiating between the two conditions requires careful evaluation of developmental history and behavioral symptoms. Both conditions can benefit from tailored interventions, including behavioral therapy and social skills training.
Conduct Disorder and DMDD
DMDD shares some characteristics with conduct disorder, particularly aggressive behavior and defiant behavior. However, conduct disorder involves more severe antisocial behaviors, such as aggression toward people.
Identifying these distinctions is vital for developing appropriate intervention strategies. Tailoring interventions based on specific behavioral patterns ensures more effective treatment.


DMDD and Sensory Processing Disorder
Sensory processing challenges may be present in children with DMDD. These challenges lead to heightened irritability and severe reactions to environmental stimuli.
Addressing these sensory challenges through sensory integration therapy may reduce irritability. Managing sensory sensitivities can play a crucial role in improving overall functioning.
Strategies for Reducing Temper Tantrums in Children
Strategies for reducing temper tantrums in children with DMDD include consistent behavioral interventions. Positive reinforcement techniques are also important.
Cognitive-behavioral therapy for mood disorders in children can be effective in teaching emotional regulation skills. Parent training helps implement these strategies at home, reducing severe temper tantrums and overall irritability.
Technological Advances in DMDD Treatment
Recent advancements in technology offer new ways to support children with DMDD. Virtual reality and biofeedback are emerging tools to teach self-regulation skills.
These technologies, combined with traditional approaches like cognitive-behavioral therapy, offer promising avenues. They help enhance emotional regulation and reduce disruptive symptoms.
DMDD and Vitamin Deficiency
Emerging research suggests a link between DMDD and vitamin deficiency. Deficiencies in vitamin D and B vitamins may contribute to irritable mood symptoms.
Addressing these deficiencies may help manage symptoms and improve overall mental health. Dietary assessments can be integrated into treatment plans to support better outcomes.
DMDD and Non-Motor Symptoms
Non-motor symptoms such as sleep disturbances are common in children with DMDD. Fatigue can also exacerbate irritability and contribute to emotional dysregulation.
Addressing non-motor symptoms through a comprehensive treatment approach may improve mood stability. This holistic approach helps enhance overall functioning.
Field Trials and Clinical Trials on DMDD
Field trials and clinical trials continue to provide valuable insights into DMDD. These trials help refine diagnostic criteria, understand prevalence rates, and identify effective treatment strategies.
Contributions from researchers such as Waxmonsky et al. and Costello EJ have been instrumental. Their work advances knowledge on disruptive mood dysregulation disorder.


Early Signs of Disruptive Mood Dysregulation Disorder
Early signs of disruptive mood dysregulation disorder include frequent and severe temper outbursts. Persistent irritability and difficulty coping with frustration are also common.
Recognizing these signs in young children is essential for early intervention. Early treatment can reduce the severity of symptoms and improve developmental outcomes.
DMDD and Risk of Developing Depression
Children with DMDD are at an increased risk of developing depression later in life. Persistent negative mood and irritability-related impairment contribute to depressive symptoms.
Monitoring and early intervention are crucial to reduce the risk of long-term mental health issues. Comprehensive care can mitigate risks and enhance well-being.
DMDD and Emotional Regulation Skills
Building emotional regulation skills is a core component of therapy for children with DMDD. Techniques such as cognitive-behavioral therapy are used to help children manage irritable mood symptoms effectively.
Mindfulness can also play a role in strengthening emotional regulation skills. Reducing the frequency and intensity of angry outbursts is a key goal.
DMDD and Academic Accommodations
Children with DMDD often require specific academic accommodations. Interventions like Individualized Education Programs (IEPs) can provide necessary support.
These accommodations help manage outburst symptoms and improve academic performance. School-based interventions aim to create a supportive learning environment.
DMDD and Functional Outcomes
Functional outcomes for children with DMDD vary based on the effectiveness of early intervention. Comprehensive treatment, including parent training, therapy, and school support, improves chances of positive outcomes.
Monitoring progress and adjusting interventions are key to ensuring the best developmental trajectory. Early and consistent support can lead to better functional outcomes.
DMDD and Anger Management Techniques
Anger management techniques help children with DMDD cope with emotional dysregulation. Techniques like relaxation exercises and cognitive restructuring are commonly used.
Role-playing can also assist in managing aggressive behavior. These strategies, often integrated into cognitive-behavioral therapy, enhance emotional regulation and reduce irritable behaviors.
DMDD and Peer Interactions
DMDD significantly affects peer interactions. The irritable mood and frequent temper tantrums can lead to difficulties in forming friendships.
Social skills training and structured group activities can help children improve peer interactions. Building lasting relationships requires support and practice in social settings.
DMDD and Language Development
Language development may be impacted in children with DMDD. Frequent outbursts and difficulties in regulating emotions can interfere with effective communication.
Targeted interventions, such as speech and language therapy, aid in improving communication skills. This can enhance social interactions and help children express emotions appropriately.
DMDD and Suicide Ideation
Children and adolescents with DMDD may be at increased risk for suicide ideation. Persistent irritability and negative mood are major risk factors.
Early and comprehensive intervention, involving both psychotherapy and family support, is crucial. Providing a supportive environment is essential for reducing the risk of self-harm.


Parent Support Groups for Disruptive Mood Dysregulation Disorder
Parent support groups provide invaluable assistance for managing DMDD. Connecting with other parents helps in managing irritable mood symptoms and aggressive behaviors.
Support groups also offer resources and coping strategies for parents. Engaging in these groups can ultimately enhance family resilience and improve outcomes.
Intramural Research Program on DMDD
The Intramural Research Program at the National Institute of Mental Health actively investigates the factors contributing to DMDD. Their research focuses on both neurobiological and environmental aspects.
These studies aim to refine diagnostic criteria and identify early indicators of DMDD. Continued research may lead to better understanding and improved functional outcomes for affected children.
Conclusion
Disruptive Mood Dysregulation Disorder represents an important advancement in our understanding of chronic irritability and severe temper outbursts in children and adolescents. As research in this area continues to grow, it is hoped that improved diagnostic accuracy and targeted interventions will lead to better outcomes for affected individuals and their families.
From Embrace Inner Chaos to your inbox
Transform your Chaos into authentic personal growth – sign up for our free weekly newsletter! Stay informed on the latest research advancements covering:
Narcissistic Personality Disorder (NPD)
Frequently Asked Questions
What Are the Key Symptoms of Disruptive Mood Dysregulation Disorder?
Disruptive Mood Dysregulation Disorder (DMDD) primarily manifests as severe, recurrent temper outbursts that are grossly out of proportion to the situation. These outbursts can include verbal rages or physical aggression, occurring at least three times per week.
Besides these outbursts, children with DMDD display a persistently irritable or angry mood most of the day, nearly every day. According to the American Academy of Child and Adolescent Psychiatry, DMDD symptoms significantly affect children’s social, academic, and emotional functioning.
How Is Disruptive Mood Dysregulation Disorder Diagnosed?
The diagnosis of DMDD requires a thorough clinical evaluation, including a review of the child’s medical history and observable behavior patterns. A child must exhibit severe temper outbursts inconsistent with their developmental level, occurring frequently for at least one year.
The irritability must be present in multiple settings such as at home, school, or with peers. According to Mayo Clinic, it is important that these symptoms are not better explained by other mental disorders like bipolar disorder or autism spectrum disorder.
How Does DMDD Differ From Bipolar Disorder in Youth?
DMDD is often confused with bipolar disorder, but significant differences exist between these conditions. Bipolar disorder involves episodes of mania or hypomania, characterized by elevated or expansive moods.
DMDD focuses on chronic irritability and severe temper outbursts without manic episodes. According to Johns Hopkins Medicine, differentiating between these conditions is crucial for appropriate treatment.
What Are the Common Comorbidities Associated With DMDD?
Children with DMDD often present with other mental health conditions, with attention-deficit/hyperactivity disorder (ADHD) being one of the most common comorbidities. Additionally, anxiety disorders and conduct disorders are frequently observed alongside DMDD.
These comorbidities complicate the clinical picture, making effective treatment planning critical. The National Institute of Mental Health reports that addressing comorbid conditions simultaneously is key to improving outcomes for affected children.
What Treatment Options Are Available for DMDD?
The treatment for DMDD involves a combination of behavioral interventions and, in some cases, pharmacological treatment. Cognitive-behavioral therapy (CBT) is commonly used to help children develop coping skills and manage negative emotions.
Parent training and family therapy can also support families in dealing with severe mood dysregulation. In some cases, medication like stimulants or antidepressants may be prescribed. The American Psychological Association emphasizes the importance of an individualized treatment plan.
How Effective Is Cognitive-Behavioral Therapy in Treating DMDD?
Cognitive-behavioral therapy (CBT) has shown promising results in treating DMDD by targeting the child’s emotional responses. It teaches them coping mechanisms for irritability and outbursts.
CBT helps children recognize triggers for their temper tantrums and develop skills to handle frustrating situations calmly. According to Child Mind Institute, CBT is effective when paired with consistent parental involvement.
Can DMDD Be Managed Without Medication?
While medication can be part of a treatment plan for DMDD, non-pharmacological approaches have also been successful. Psychotherapy, particularly cognitive-behavioral therapy, parent training programs, and family therapy have been effective in managing disruptive behaviors.
According to WebMD, behavior management strategies that include consistency, structure, and positive reinforcement can significantly help. Many children manage DMDD symptoms effectively without relying on medications.
How Does DMDD Impact Family Dynamics?
DMDD can significantly affect family dynamics, as parents often face challenges in managing chronic irritability and severe tantrums. This leads to high levels of stress within the household.
Siblings may also feel neglected or become targets of the outbursts, further complicating family relationships. As highlighted by Verywell Family, parents may experience higher rates of anxiety and depression due to these challenges.
What Role Do Pediatricians Play in Diagnosing DMDD?
Pediatricians are often the first point of contact when parents notice severe mood dysregulation or frequent temper outbursts. Pediatricians conduct preliminary assessments and refer children to specialists for comprehensive evaluations.
According to Cleveland Clinic, pediatricians also monitor coexisting medical conditions that could contribute to mood dysregulation. They offer guidance on behavioral management strategies in school and home settings.
How Does DMDD Affect Academic Performance?
Children with DMDD often struggle academically due to difficulty managing anger and irritability. This may lead to conflicts with teachers and peers.
Chronic irritability can result in a lack of focus and difficulty in completing schoolwork, affecting learning outcomes. As reported by Edutopia, school-based interventions can improve academic performance by providing emotional support.
What Are the Long-Term Outcomes for Children Diagnosed With DMDD?
Long-term outcomes for children with DMDD can vary. Some children show improvement with consistent treatment, while others continue to experience difficulties into adolescence and adulthood.
According to Boston Children’s Hospital, early intervention, including therapeutic and educational measures, greatly increases the likelihood of better outcomes. It reduces the risk of developing anxiety or other mood disorders later.
How Is DMDD Related to Severe Mood Dysregulation?
DMDD is related to severe mood dysregulation, a concept introduced to describe children with chronic irritability and frequent temper outbursts. Severe mood dysregulation has similarities to DMDD but was defined more clearly through specific diagnostic criteria in DSM-5.
According to Psychiatry Online, DMDD focuses on behavioral symptoms and temper outbursts. Severe mood dysregulation included a broader range of non-specific symptoms like increased arousal.
What Are the Differences Between DMDD and Oppositional Defiant Disorder (ODD)?
Both DMDD and Oppositional Defiant Disorder (ODD) involve temper outbursts and defiance. However, DMDD is characterized by pervasive irritability that negatively impacts multiple settings of life.
Unlike ODD, which is often limited to oppositional behaviors, DMDD involves intense and persistent irritability. According to Healthline, understanding these differences is crucial for treatment.
How Do Parent Training Programs Help in Managing DMDD?
Parent training programs provide parents with tools to effectively manage severe irritability and outbursts. Techniques like positive reinforcement and structured daily routines help reduce negative interactions.
According to Parenting Science, these sessions also focus on helping parents understand triggers for their child’s outbursts. This ultimately contributes to a calmer home environment.
Can DMDD Lead to Other Mental Health Issues in Adolescence?
Children diagnosed with DMDD are at increased risk of developing anxiety and depressive disorders in adolescence. Chronic irritability increases the likelihood of experiencing negative mental health outcomes.
According to Stanford Medicine, long-term studies indicate that ongoing treatment can mitigate these risks. Involvement of parents and schools is crucial in a child’s treatment plan.
What Are Some Strategies for Reducing Temper Outbursts in Children With DMDD?
Effective strategies for reducing temper outbursts include implementing consistent routines and reinforcing positive behaviors. These strategies help children predict their environment and respond to stressors more adaptively.
According to KidsHealth, mindfulness and relaxation exercises can also be helpful. These techniques allow children to manage their reactions more effectively when overwhelmed.
How Does DMDD Affect Social Relationships in Children?
DMDD can profoundly impact a child’s social relationships. Chronic irritability and frequent outbursts make it challenging for children to form and maintain friendships.
According to Child Trends, children with DMDD are more likely to be rejected by peers and may struggle with loneliness. Social skills training can improve these relationships significantly.
How Do Neurobiological Factors Contribute to DMDD?
Research suggests that neurobiological factors, including irregularities in brain areas involved in emotion regulation, may contribute to DMDD. These include the amygdala and prefrontal cortex.
According to Brain & Behavior Research Foundation, children with DMDD may have differences in brain activity. This can explain their heightened irritability and reactivity.
Are There Cultural Considerations in the Diagnosis of DMDD?
Cultural differences play a significant role in the diagnosis of DMDD. Perceptions of irritability and acceptable behavior vary across cultures.
According to American Psychiatric Association, what is considered extreme in one culture may be seen as normal in another. Clinicians must consider cultural norms to ensure an accurate diagnosis.
How Can School-Based Interventions Help Children With DMDD?
School-based interventions focus on providing emotional and behavioral support within the educational setting. These interventions include individualized behavior plans and counseling services.
According to National Education Association, school-based support can help improve both academic performance and social functioning. Consistent care across environments is vital for managing DMDD symptoms effectively.




