Last updated on December 18th, 2024 at 03:12 am
- 1. The Complex Relationship Between PTSD and Sleep
- 1.1 The Vicious Cycle of PTSD and Sleep Disorders
- 2. Understanding PTSD Nightmares
- 2.1 Characteristics of PTSD Nightmares
- 2.2 The Persistence of PTSD Nightmares
- 3. The Impact of PTSD Nightmares on Daily Life
- 3.1 Mental Health Consequences
- 3.2 Relationship and Social Impacts
- 3.3 Occupational and Functional Impairment
- 4. Treatment Approaches for PTSD Nightmares
- 4.1 Psychotherapeutic Interventions
- 4.2 Medication Options
- 5. Strategies for Preventing and Coping with PTSD Nightmares
- 5.1 Sleep Hygiene and Environment
- 5.2 Nightmare Coping Techniques
- 5.3 Lifestyle Factors
- 6. The Future of PTSD Nightmare Treatment
- The Role of REM Sleep in PTSD-Related Sleep Disturbances
- Trauma-Induced Sleep Deprivation and Melatonin Production
- PTSD Nightmare Interventions and Therapeutic Approaches
- The Impact of PTSD on Sleep Architecture
- Relations Between Sleep Problems and Mental Disorders in PTSD
- Disturbances in Adults: Nocturnal Behaviors and Movements During Sleep
- Sleep Apnea and Trauma-Induced Sleep Disorders
- Clinical Relevance of Treating PTSD-Related Sleep Disorders
- Trauma-Induced Sleep Evaluations: Identifying Disordered Sleep
- PTSD and Circadian Rhythm Disturbances
- Nightmare Frequency and Severity: Addressing Trauma-Related Nightmares
- Future Studies and Research Directions
- Trauma-Induced Sleep Enhancements and Rehabilitation Strategies
- Impact of Trauma-Related Insomnia on Daytime Sleepiness
- PTSD-Related Nocturnal Behaviors and Hypnagogic Hallucinations
- Cognitive Therapy and Trauma-Induced Sleep Problems
- Treatment of Nightmare Disorder and Trauma-Related Sleep Issues
- Night Terrors and PTSD-Associated Sleep Disorders
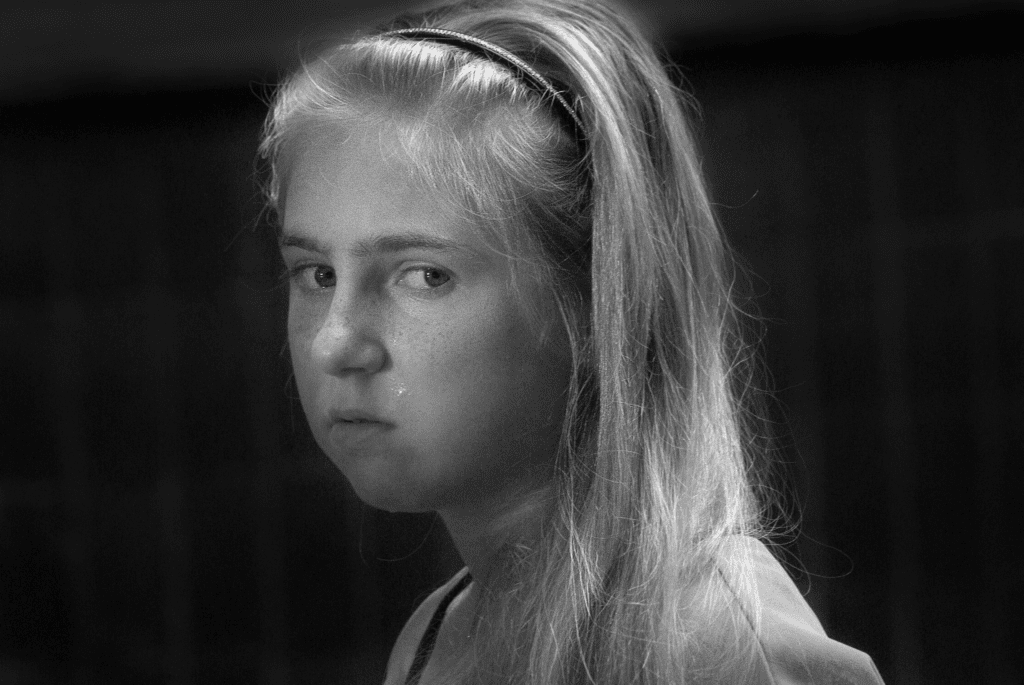
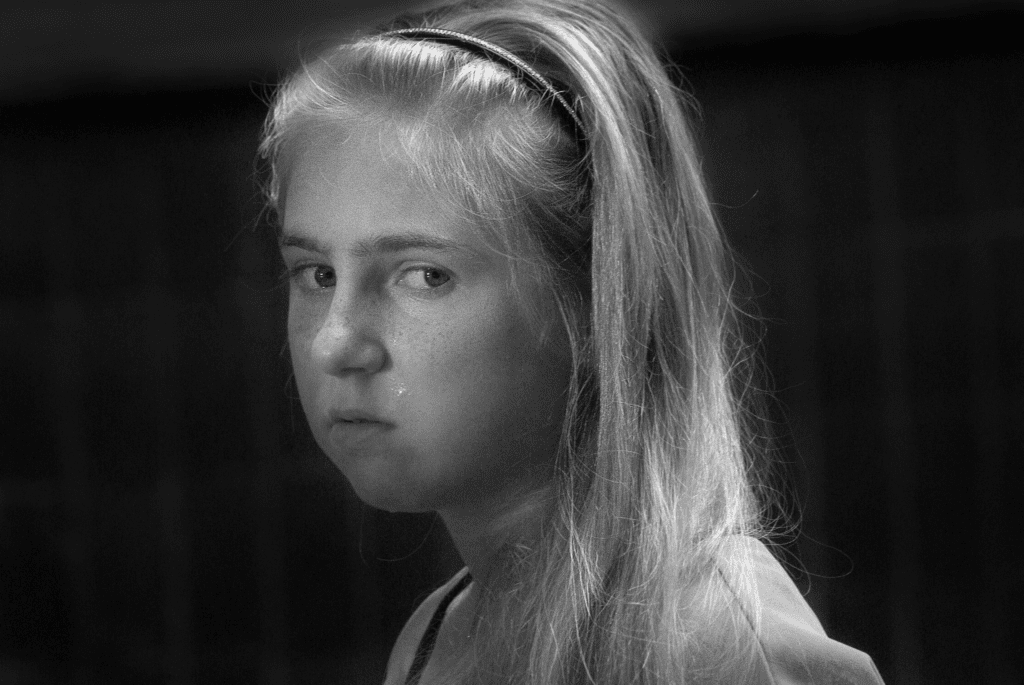
- Adverse Childhood Experiences and PTSD Sleep Quality
- Trauma-Induced Sleep Recovery and Clinical Care Approaches
- The Role of Selective Serotonin Reuptake Inhibitors in Sleep Quality
- Sleep Variables and Improvements in PTSD-Associated Nightmares
- Trauma-Induced Sleep Disorder Treatments and Military-Related PTSD
- Conclusion
- Frequently Asked Questions
- How Does Post-Traumatic Stress Disorder Affect Sleep?
- What Are PTSD Nightmares and How Do They Differ From Regular Nightmares?
- Why Are PTSD Nightmares Considered a Symptom of Post-Traumatic Stress Disorder?
- How Does Cognitive-Behavioral Therapy Help With PTSD Nightmares?
- What Role Does Imagery Rehearsal Therapy Play in Treating PTSD Nightmares?
- How Does PTSD Contribute to Poor Sleep Quality in Individuals?
- How Are PTSD Nightmares Different From Trauma-Related Nightmares?
- What Are the Effects of Trauma-Related Nightmares on Daytime Functioning?
- How Does REM Sleep Disruption Relate to PTSD Nightmares?
- Are There Pharmacological Treatments for PTSD Nightmares?
- How Does Fear of Sleep Develop in PTSD Patients?
- What Are the Impacts of Daytime Sleepiness on PTSD Symptom Severity?
- How Effective Are Selective Serotonin Reuptake Inhibitors in Reducing PTSD Nightmares?
- What Is the Role of REM Sleep Behavior Disorder in PTSD?
- What Techniques Help in Improving PTSD-Related Sleep Quality?
- How Are Nocturnal Behaviors Affected by PTSD?
- How Do Sleep Terrors Differ From PTSD Nightmares?
- How Does Obstructive Sleep Apnea Influence PTSD Nightmares?
- Are PTSD Nightmares More Common in Military Personnel?
- How Can Cognitive Therapy Help With PTSD-Induced Sleep Problems?
Post-traumatic stress disorder (PTSD) can have profound effects on sleep, with nightmares being one of the most distressing and persistent symptoms. Up to 72% of individuals with PTSD experience recurring nightmares that can persist for years, even after other symptoms have improved.
These nightmares not only disrupt sleep but can exacerbate other PTSD symptoms and significantly impact quality of life. Let’s understand how PTSD nightmares impacts sleep, causes distressing dreams, and explore solutions to regain restful nights and manage stress effectively.
1. The Complex Relationship Between PTSD and Sleep
Sleep is essential for physical and mental wellbeing, but obtaining restful sleep can be a major challenge for those with PTSD. Research suggests that PTSD and nightmares involve altered activity in overlapping regions of the brain, though the exact relationship is not fully understood. Compared to those without PTSD, individuals with the disorder tend to have poorer overall sleep quality, including:
- Reduced total sleep time
- Increased nighttime awakenings
- Difficulties falling and staying asleep
- Less time spent in restorative deep sleep stages
A typical night’s sleep consists of multiple cycles through different sleep stages, including rapid eye movement (REM) and non-REM sleep. While PTSD-related nightmares can occur during any stage, they tend to be more frequent during the latter part of the night when REM sleep is more prevalent. These disruptions lead to chronic sleep deprivation and feelings of helplessness.
1.1 The Vicious Cycle of PTSD and Sleep Disorders
PTSD and sleep disorders often create a vicious cycle – PTSD symptoms make it difficult to sleep, while lack of sleep exacerbates PTSD symptoms. This complex interplay means that effectively treating one condition requires addressing both. Beyond the psychological toll, chronic sleep deprivation due to PTSD nightmares can increase risks for serious health issues like:
- Obesity
- Cardiovascular disease
- Type 2 diabetes
- Weakened immune function
- Cognitive impairment
- Mood disorders
2. Understanding PTSD Nightmares
Nightmares are considered a hallmark symptom of PTSD. While typical nightmares may feel extreme, they are usually not related to actual events. In contrast, PTSD nightmares often directly replay traumatic experiences in vivid detail. For combat veterans, this may involve reliving battlefield horrors. For civilian trauma survivors, it could mean re-experiencing assaults, accidents, or disasters.
2.1 Characteristics of PTSD Nightmares
PTSD nightmares tend to have several distinguishing features:
- Intense sensory experiences (sights, sounds, smells, physical sensations)
- Extreme emotions like terror, helplessness, or rage
- Repetitive themes or exact replays of traumatic events
- A sense of immediate, life-threatening danger
- Difficulty distinguishing the nightmare from reality upon waking
These nightmares can be so terrifying that many individuals develop a fear of sleep itself, further compounding sleep difficulties. The chronic sleep deprivation that results impacts all areas of life – work performance, relationships, physical health, and emotional wellbeing.
2.2 The Persistence of PTSD Nightmares
One of the most challenging aspects of PTSD nightmares is their persistence. While daytime PTSD symptoms may improve with time and treatment, nightmares often continue for years or even decades after the original trauma. This can leave survivors feeling hopeless and wondering if they’ll ever find relief.
Additionally, once nightmares become established, they can accelerate the progression of PTSD. The ongoing nightly trauma reinforces fear responses and keeps the brain in a hypervigilant state. This makes it more difficult for individuals to process and integrate their traumatic experiences.


3. The Impact of PTSD Nightmares on Daily Life
The effects of PTSD nightmares extend far beyond disrupted sleep. Chronic nightmares can have wide-ranging impacts on mental health, relationships, and overall functioning.
3.1 Mental Health Consequences
Persistent nightmares take a severe toll on mental health and wellbeing. Common effects include:
- Increased anxiety and hypervigilance
- Depression and feelings of hopelessness
- Irritability and mood swings
- Difficulty concentrating and memory problems
- Emotional numbing or detachment
- Increased risk of substance abuse as a coping mechanism
Most alarmingly, individuals with PTSD who experience frequent nightmares are at significantly higher risk for suicidal thoughts and behaviors. One study found the risk of suicidal ideation was three times higher in this group.
3.2 Relationship and Social Impacts
PTSD nightmares can strain relationships and social connections in several ways:
- Sleep disturbances affecting bed partners
- Irritability and mood swings causing conflicts
- Social withdrawal due to fatigue or embarrassment
- Difficulty being emotionally available to loved ones
- Strain on intimate relationships due to nightmares’ content
3.3 Occupational and Functional Impairment
Chronic sleep deprivation from PTSD nightmares often leads to:
- Reduced work performance and productivity
- Increased absenteeism
- Higher risk of workplace accidents
- Difficulty pursuing education or career goals
- Challenges with daily tasks and responsibilities
4. Treatment Approaches for PTSD Nightmares
While PTSD nightmares can feel intractable, several evidence-based treatments have shown promise in reducing their frequency and intensity. A comprehensive treatment plan often involves a combination of therapeutic approaches and, in some cases, medication.
4.1 Psychotherapeutic Interventions
Several types of psychotherapy have demonstrated effectiveness for PTSD nightmares:
Image Rehearsal Therapy (IRT)
IRT is considered a first-line treatment for post-traumatic nightmares. This approach involves:
- Writing down recurring nightmares in detail
- Modifying the nightmare script to create a new, less distressing ending
- Mentally rehearsing the new version daily
- Gradually replacing the traumatic imagery with more positive alternatives
Studies have shown that 60-70% of individuals experience significant reductions in nightmare frequency and distress with IRT.


Cognitive Behavioral Therapy for Insomnia (CBT-I)
CBT-I helps address the sleep disturbances associated with PTSD nightmares. Key components include:
- Sleep hygiene education
- Stimulus control techniques
- Sleep restriction therapy
- Cognitive restructuring of sleep-related thoughts
- Relaxation training
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is an established treatment for PTSD that can also help with nightmares. It involves:
- Recalling traumatic memories while performing guided eye movements
- Processing and integrating traumatic experiences
- Reducing emotional distress associated with trauma memories
4.2 Medication Options
While psychotherapy is generally the first-line approach, certain medications may be helpful in managing PTSD nightmares:
Prazosin
Originally developed as a blood pressure medication, prazosin has shown promise in reducing PTSD nightmares. It works by blocking norepinephrine, a stress hormone that may contribute to nightmares. Studies have found prazosin can:
- Decrease nightmare frequency and intensity
- Improve overall sleep quality
- Reduce daytime PTSD symptoms
Other Medications
While research is more limited, other medications that have shown potential benefit for some individuals include:
- Antidepressants (e.g., SSRIs like sertraline or paroxetine)
- Atypical antipsychotics (e.g., risperidone)
- Anticonvulsants (e.g., topiramate)
- Alpha-agonists (e.g., clonidine)
5. Strategies for Preventing and Coping with PTSD Nightmares
In addition to professional treatment, there are several self-help strategies individuals can use to reduce the impact of PTSD nightmares:
5.1 Sleep Hygiene and Environment
- Establish a consistent sleep schedule
- Create a calm, comfortable sleep environment
- Avoid caffeine, alcohol, and heavy meals before bed
- Limit screen time in the evening
- Practice relaxation techniques like deep breathing or progressive muscle relaxation


5.2 Nightmare Coping Techniques
- Keep a nightmare journal to identify patterns and triggers
- Practice grounding techniques upon waking from a nightmare
- Use positive imagery or calming thoughts before sleep
- Engage in gentle physical activity if unable to fall back asleep
5.3 Lifestyle Factors
- Regular exercise (but not too close to bedtime)
- Stress management techniques like mindfulness or yoga
- Avoiding substance use as a coping mechanism
- Building a strong support network
- Engaging in meaningful daytime activities
6. The Future of PTSD Nightmare Treatment
Research into PTSD and nightmare treatment continues to evolve. Some promising areas of investigation include:
- Virtual reality exposure therapy for trauma processing
- Neurofeedback and brain stimulation techniques
- Combination therapies integrating multiple treatment modalities
- Personalized medicine approaches based on genetic and neurobiological factors
- Novel pharmacological targets for nightmare reduction
As our understanding of the neurobiology of PTSD and sleep deepens, more targeted and effective treatments are likely to emerge. For now, a comprehensive approach combining evidence-based therapies, medication when appropriate, and lifestyle modifications offers the best hope for those suffering from PTSD nightmares.
The Role of REM Sleep in PTSD-Related Sleep Disturbances
REM sleep is crucial for emotional processing and memory consolidation. However, individuals with post-traumatic stress disorder often experience PTSD and REM sleep disruption.
Trauma-induced sleep issues commonly manifest as changes in REM sleep, which may contribute to intense nightmares and frequent awakenings. Increased emotional intensity during REM cycles often leads to more vivid traumatic nightmares, reinforcing sleep difficulties and exacerbating PTSD symptoms.
Trauma-Induced Sleep Deprivation and Melatonin Production
PTSD impacts sleep in various ways, including changes in melatonin production. The disruption of circadian rhythms leads to difficulty falling asleep and remaining in deep sleep, contributing to trauma-induced sleep deprivation.
Studies have linked reduced melatonin levels to disturbances in adults with PTSD, suggesting that targeted interventions might help restore sleep patterns. Natural methods to regulate melatonin production, such as strict sleep schedules and light exposure management, are considered valuable elements of PTSD sleep hygiene practices.
PTSD Nightmare Interventions and Therapeutic Approaches
Addressing PTSD nightmares often requires specific PTSD nightmare therapy approaches. Imagery rehearsal therapy, a cognitive-behavioral treatment, focuses on modifying trauma-related nightmares to reduce their frequency and severity.
This intervention helps change the narrative of traumatic nightmares, thereby improving overall sleep quality. Experimental studies have also explored the use of selective serotonin reuptake inhibitors, indicating potential improvements in sleep quality and PTSD symptom reduction.
The Impact of PTSD on Sleep Architecture
Trauma-induced sleep disorders have a profound effect on sleep architecture, which refers to the distribution of sleep stages across the night. PTSD-related sleep disorders often result in a reduction of restorative deep sleep stages while increasing periods of light sleep and disturbed sleep.
Such changes impact subjective sleep quality and lead to poor sleep quality overall. Disrupted sleep architecture also results in increased nighttime symptoms, making it difficult for individuals to recover effectively from traumatic events.
Relations Between Sleep Problems and Mental Disorders in PTSD
Sleep difficulties are a common symptom of PTSD, and their effects on mental disorders can be severe. There is a well-established temporal relationship between PTSD and other psychiatric disorders, such as depression and anxiety.
Chronic disturbances in adults lead to a secondary symptom: the persistence of poor mental health. Addressing sleep issues with effective treatment of PTSD is often crucial for improving daytime symptoms and the individual’s overall well-being.
Disturbances in Adults: Nocturnal Behaviors and Movements During Sleep
Individuals with PTSD often experience nocturnal behaviors, such as movements during sleep and vocalizations. REM sleep behavior disorder is commonly observed in those with PTSD, with frequent limb movements being a sign of disturbed sleep.
This sleep disorder can significantly impact quality sleep, as movements during sleep tend to lead to further arousals, preventing progression into deeper sleep stages. A study conducted by Germain A, noted a significant prevalence of REM sleep behavior disorder among trauma survivors.
Sleep Apnea and Trauma-Induced Sleep Disorders
PTSD and sleep apnea are often linked, particularly in veterans and individuals exposed to highly stressful environments. Trauma-induced sleep disorders, like obstructive sleep apnea, exacerbate poor sleep and lead to symptoms of PTSD becoming more severe.
Studies have shown a notable correlation between trauma-related sleep problems and obstructive sleep apnea, with individuals experiencing worsened quality sleep and fragmented rest. Treatment approaches for trauma-related insomnia solutions often include Continuous Positive Airway Pressure (CPAP) therapy to alleviate these issues.
Clinical Relevance of Treating PTSD-Related Sleep Disorders
PTSD nightmare interventions and cognitive therapy are instrumental in managing trauma-related insomnia. Clinical trials have highlighted the effectiveness of selective serotonin reuptake inhibitors and other treatment approaches to improve PTSD-associated nightmares.
According to Montgomery P’s critical review, cognitive-behavioral therapy showed promising results in enhancing subjective sleep quality and reducing sleep issues in individuals with severe PTSD symptoms.
Trauma-Induced Sleep Evaluations: Identifying Disordered Sleep
Evaluating trauma-induced sleep disorders is essential for providing effective clinical care. PTSD and sleep counseling often involve a comprehensive clinical interview and the use of health information resources to identify disordered sleep patterns.
Professionals utilize tools like polysomnography to diagnose PTSD and sleep apnea, allowing them to create tailored PTSD sleep therapy programs that aim to improve quality sleep and reduce trauma-related sleep disturbances. These programs are critical for helping individuals regain sleep quality and diminish the impact of PTSD symptoms.
PTSD and Circadian Rhythm Disturbances
Circadian rhythm disturbances are prevalent among individuals dealing with PTSD. The natural sleep-wake cycle becomes disrupted following traumatic event exposure, leading to difficulties maintaining a consistent sleep schedule.
A systematic review and meta-analysis by Mysliwiec V found significant temporal relations between PTSD symptoms and disrupted sleep-wake rhythms. Understanding how PTSD and circadian rhythm disturbances interact can help in developing strategies for restoring healthy sleep cycles.
Nightmare Frequency and Severity: Addressing Trauma-Related Nightmares
The frequency of nightmares experienced by PTSD patients has a direct correlation with the severity of their daytime symptoms. Trauma-related nightmares are often marked by their repetitive nature and strong emotional content.
Treatments for nightmare disorder, such as cognitive-behavioral therapy and prazosin, have demonstrated reductions in both the severity of nightmares and the adverse effects on overall health outcomes. Nappi CM’s placebo-controlled study revealed significant reductions in the severity of nightmares among PTSD patients who received prazosin compared to a placebo group.


Future Studies and Research Directions
Future studies should focus on PTSD and sleep research to enhance treatment outcomes. Researchers are particularly interested in improving PTSD sleep disorder management through novel interventions, such as trauma-related sleep therapy and pharmacological advancements.
Studies have been exploring virtual reality exposure therapies and personalized medicine for treating trauma-induced sleep disorders more effectively. Moreover, understanding causal relationships between traumatic stress symptoms and sleep disturbances will be vital for advancing clinical care for individuals suffering from PTSD-related sleep problems.
Trauma-Induced Sleep Enhancements and Rehabilitation Strategies
Improving sleep quality for individuals with PTSD is an ongoing challenge. Trauma-induced sleep enhancements include both pharmacological and therapeutic strategies aimed at providing relief from PTSD-induced night terrors and sleep terrors.
The American Academy of Sleep Medicine suggests adopting PTSD sleep improvement strategies, including behavioral interventions, medications like selective serotonin reuptake inhibitors, and cognitive therapy. These strategies aim to restore sleep architecture and ultimately support PTSD sleep rehabilitation and overall recovery.
Impact of Trauma-Related Insomnia on Daytime Sleepiness
Trauma-related insomnia frequently leads to daytime sleepiness, impairing overall function and daily productivity. Sleep difficulties stemming from PTSD can manifest as ongoing fatigue and reduced focus throughout the day.
Addressing insomnia symptoms and improving quality sleep is essential for enhancing daytime function. This is critical in maintaining effective performance in personal and professional environments.
PTSD-Related Nocturnal Behaviors and Hypnagogic Hallucinations
Individuals with PTSD are also prone to experiencing hypnagogic hallucinations, which occur during transitions from wakefulness to sleep. These vivid hallucinations are often tied to traumatic events and add to the severity of PTSD-related sleep disorders.
Frequent nocturnal behaviors and episodes of disturbed sleep further impact the quality of sleep, leaving individuals feeling unrested. Addressing these hallucinations and behaviors is crucial for reducing overall PTSD-related sleep difficulties.
Cognitive Therapy and Trauma-Induced Sleep Problems
Cognitive-behavioral therapy has proven effective for treating trauma-induced sleep problems, including PTSD-induced night terrors and frequent nightmares. Cognitive therapy is tailored to target re-experiencing symptoms, helping individuals challenge the thoughts that contribute to trauma-related sleep disruptions.
A study by Jenkins MM highlighted the positive outcomes in reducing PTSD nightmares with cognitive-behavioral treatment. The therapy aims to modify the thought patterns that trigger distressing sleep issues, providing long-term relief.
Treatment of Nightmare Disorder and Trauma-Related Sleep Issues
Treatment of nightmare disorder often includes a combination of medication and therapeutic approaches. Imagery rehearsal therapy is one of the most effective ways to address PTSD nightmares.
A study by Brownlow JA emphasized the role of imagery rehearsal therapy in reducing the emotional intensity of trauma nightmares. This technique helps individuals regain control over their sleep by altering the content of distressing dreams.


Night Terrors and PTSD-Associated Sleep Disorders
Night terrors are a common occurrence among individuals with PTSD, contributing to PTSD-associated nightmares and nighttime symptoms. These episodes can be marked by intense fear, vocalizations, and physical movements, further complicating the sleep environment.
Addressing night terrors is an important aspect of PTSD sleep disorder management and involves both medication and therapeutic interventions. Effective treatment can improve the sleep environment and overall sleep quality.
Adverse Childhood Experiences and PTSD Sleep Quality
Adverse childhood experiences play a significant role in the development of PTSD and subsequent sleep disturbances in adults. Trauma-related sleep patterns often originate from childhood traumas, with PTSD-induced night terrors and PTSD-related sleep disorders emerging as adults.
A systematic review by Ohayon MM found a strong link between early adverse experiences and lifelong sleep issues. Addressing these early traumas is crucial for breaking the cycle of poor sleep quality.
Trauma-Induced Sleep Recovery and Clinical Care Approaches
Trauma-induced sleep recovery requires a multifaceted approach, incorporating both clinical care and self-help strategies. Health care professionals often recommend trauma-related sleep interventions to improve subjective sleep quality and reduce trauma-induced sleep disturbances.
This approach typically involves both cognitive-behavioral treatments and medical advice aimed at promoting PTSD sleep optimization. Utilizing these combined strategies supports long-term improvements in sleep patterns.
The Role of Selective Serotonin Reuptake Inhibitors in Sleep Quality
Selective serotonin reuptake inhibitors (SSRIs) have been found effective in improving sleep quality for PTSD patients. SSRIs reduce the severity of nightmares and enhance overall sleep architecture, which aids in PTSD sleep rehabilitation.
According to a study by Hoge EA, SSRIs also contribute to improving overall PTSD treatment outcomes by enhancing sleep quality. This class of medication is often a critical component in treating both sleep and PTSD symptoms.
Sleep Variables and Improvements in PTSD-Associated Nightmares
Tracking sleep variables can help identify improvements in PTSD-associated nightmares and overall sleep quality. Monitoring sleep patterns, such as REM sleep duration and frequency of awakenings, provides insight into treatment outcomes.
Research suggests that individuals who track their sleep are more likely to observe improvements, especially when combining medication and cognitive-behavioral therapy. This approach facilitates better management of trauma-related sleep issues.
Trauma-Induced Sleep Disorder Treatments and Military-Related PTSD
Military personnel exposed to combat are at heightened risk for trauma-induced sleep disorders, including PTSD and sleep apnea. Treatments are often tailored to address military-related PTSD and include a combination of therapeutic interventions and sleep disorder therapies.
A study by Ulibarri VA highlighted the efficacy of trauma-related sleep assessments for military personnel, demonstrating significant improvements in sleep quality and reduction in PTSD symptoms. Addressing these unique needs is essential for ensuring effective recovery among veterans.


Conclusion
PTSD nightmares can be a debilitating and persistent symptom, significantly impacting sleep, mental health, and overall quality of life. However, with proper treatment and support, many individuals find relief and are able to reclaim restful sleep. A multifaceted approach addressing both the underlying trauma and sleep disturbances is often most effective.
It’s crucial for those experiencing PTSD nightmares to seek professional help and not suffer in silence. With ongoing research and expanding treatment options, there is hope for better sleep and healing from trauma. By addressing PTSD nightmares, individuals can take an important step towards overall recovery and improved wellbeing.
From Embrace Inner Chaos to your inbox
Transform your Chaos into authentic personal growth – sign up for our free weekly newsletter! Stay informed on the latest research advancements covering:
Narcissistic Personality Disorder (NPD)
Frequently Asked Questions
How Does Post-Traumatic Stress Disorder Affect Sleep?
Post-traumatic stress disorder (PTSD) has significant impacts on sleep, leading to frequent nightmares and disrupted sleep patterns. Individuals experiencing PTSD often endure disturbed sleep due to the re-experiencing symptoms of their traumatic events.
According to the American Psychiatric Association, this repetitive intrusion of traumatic memories into sleep results in decreased quality sleep. This can further contribute to symptoms like daytime fatigue, anxiety, and even an increased fear of sleep.
What Are PTSD Nightmares and How Do They Differ From Regular Nightmares?
PTSD nightmares, also known as post-traumatic nightmares, are distressing dreams directly related to the traumatic events a person has experienced. Unlike regular nightmares, which may not have any apparent trigger, PTSD nightmares are vivid replays of the trauma, often with intense emotional responses.
Research from the Department of Defense shows that these nightmares not only affect the quality of sleep but can also heighten the intensity of other PTSD-related symptoms. This often leads to a decrease in overall mental well-being.
Why Are PTSD Nightmares Considered a Symptom of Post-Traumatic Stress Disorder?
PTSD nightmares are considered a core symptom of PTSD because they vividly recreate traumatic experiences, contributing to sleep difficulties. According to National Library of Medicine, these nightmares represent a re-experiencing symptom, which is a hallmark of PTSD.
By repeatedly forcing sufferers to relive their trauma during sleep, these nightmares contribute to increased anxiety, insomnia, and fear of sleep. This greatly complicates recovery from PTSD.
How Does Cognitive-Behavioral Therapy Help With PTSD Nightmares?
Cognitive-behavioral therapy (CBT) is a frontline treatment for PTSD, including PTSD-related nightmares. CBT aims to help patients reframe their traumatic memories, reduce their emotional intensity, and thus decrease the frequency and severity of nightmares.
American Academy of Sleep Medicine notes that a specific form of CBT, called Imagery Rehearsal Therapy, has shown positive outcomes in reducing both nightmare intensity and overall PTSD symptoms. It encourages individuals to mentally re-script the nightmare in less distressing ways.
What Role Does Imagery Rehearsal Therapy Play in Treating PTSD Nightmares?
Imagery Rehearsal Therapy (IRT) is an effective intervention specifically targeting PTSD nightmares. It involves mentally rehearsing a more positive version of the traumatic dream while awake to reduce the emotional distress associated with the nightmare.
A study published by Nat Sci Sleep found that participants undergoing IRT experienced significant improvements in sleep quality. There was also a reduction in trauma-related sleep disturbances, which greatly improved their overall PTSD treatment outcomes.
How Does PTSD Contribute to Poor Sleep Quality in Individuals?
PTSD severely affects sleep quality due to frequent awakenings, increased arousal, and re-experiencing symptoms during sleep. These symptoms can lead to chronic insomnia, fragmented sleep, and a reduction in restorative sleep stages.
Mayo Clinic reports that these disruptions contribute to daytime symptoms like irritability, reduced concentration, and fatigue. This further complicates an individual’s ability to cope with everyday stressors.
How Are PTSD Nightmares Different From Trauma-Related Nightmares?
PTSD nightmares are a specific type of trauma-related nightmare characterized by the vivid re-experiencing of traumatic events. Trauma-related nightmares may also occur without a PTSD diagnosis and do not always involve reliving the traumatic experience itself.
According to the American Psychological Association, trauma-related nightmares can involve symbols or themes related to trauma but do not necessarily recreate the actual events. This makes PTSD nightmares more severe and distressing.
What Are the Effects of Trauma-Related Nightmares on Daytime Functioning?
Trauma-related nightmares significantly impact daytime functioning by causing increased sleep disturbances, decreased sleep duration, and heightened anxiety. The Sleep Foundation indicates that individuals experiencing these nightmares often suffer from increased daytime sleepiness and difficulty focusing on tasks.
This ultimately lowers productivity and overall mental health outcomes. Additionally, these sleep disruptions can worsen other PTSD symptoms, creating a complex cycle of distress and impairment.
How Does REM Sleep Disruption Relate to PTSD Nightmares?
Disruption in REM sleep is closely linked with PTSD nightmares, as REM sleep is the stage where dreams commonly occur. PTSD often leads to increased arousal during REM, preventing individuals from completing a full sleep cycle and leading to fragmented sleep.
A Harvard Medical School study found that patients with PTSD exhibit abnormalities in REM sleep architecture. This includes increased frequency of awakening during REM, which contributes to the persistence of trauma-related nightmares.


Are There Pharmacological Treatments for PTSD Nightmares?
Several pharmacological treatments are available for managing PTSD nightmares, including the use of selective serotonin reuptake inhibitors (SSRIs). These medications can help regulate sleep patterns and reduce the severity of nightmares.
MedlinePlus suggests that SSRIs have been effective in mitigating nightmare frequency and improving sleep quality in PTSD patients. However, individual responses to these medications can vary, and they are often used alongside other therapies like CBT.
How Does Fear of Sleep Develop in PTSD Patients?
Fear of sleep often develops in PTSD patients due to the anticipation of experiencing distressing nightmares, leading to intentional sleep avoidance. This fear can become chronic, resulting in insomnia and further deteriorating mental health.
According to Stanford Health Care, sleep avoidance not only exacerbates PTSD symptoms but also leads to a vicious cycle of poor sleep quality, increased anxiety, and impaired daytime functioning.
What Are the Impacts of Daytime Sleepiness on PTSD Symptom Severity?
Daytime sleepiness can significantly increase the severity of PTSD symptoms, affecting cognitive functioning, mood regulation, and overall resilience. The Cleveland Clinic highlights that daytime sleepiness resulting from disturbed sleep is associated with increased reactivity to stressors.
It also reduces the ability to manage symptoms such as flashbacks and hypervigilance, complicating the recovery process for PTSD patients.
How Effective Are Selective Serotonin Reuptake Inhibitors in Reducing PTSD Nightmares?
Selective serotonin reuptake inhibitors (SSRIs) are commonly used to reduce the frequency and severity of PTSD nightmares. According to Johns Hopkins Medicine, SSRIs like paroxetine and sertraline have demonstrated efficacy in minimizing nightmare episodes and improving overall sleep quality.
These medications work by reducing the arousal state associated with trauma memories. However, they are most effective when used in conjunction with other therapeutic approaches.
What Is the Role of REM Sleep Behavior Disorder in PTSD?
REM sleep behavior disorder (RBD) involves acting out dreams during REM sleep and has been observed in individuals with PTSD. RBD contributes to further disruptions in sleep as the person may perform sudden movements or vocalizations.
Mount Sinai Health System explains that RBD, when co-occurring with PTSD, increases the risk of injury during sleep. This contributes to the overall reduction in sleep quality, complicating the treatment process for PTSD.
What Techniques Help in Improving PTSD-Related Sleep Quality?
Several techniques, including cognitive-behavioral therapy, sleep hygiene practices, and relaxation exercises, have proven effective in improving sleep quality for individuals with PTSD. The National Center for PTSD suggests that implementing structured sleep routines and reducing caffeine intake can improve subjective sleep quality.
Additionally, using relaxation methods like deep breathing exercises can reduce PTSD-related sleep issues over time.
How Are Nocturnal Behaviors Affected by PTSD?
Nocturnal behaviors, including frequent awakenings and intense nightmares, are commonly affected by PTSD. These behaviors often involve distressing dreams that increase nighttime arousal and disrupt sleep cycles.
According to Harvard Health Publishing, PTSD patients exhibit more nocturnal activity and disrupted sleep patterns. This can contribute to both poor sleep quality and increased daytime symptoms such as hypervigilance and irritability.
How Do Sleep Terrors Differ From PTSD Nightmares?
Sleep terrors and PTSD nightmares differ in terms of their causes and manifestations. Sleep terrors, unlike PTSD nightmares, do not involve the vivid recall of specific traumatic events and are generally experienced during non-REM sleep.
Mayo Clinic notes that sleep terrors are characterized by extreme arousal, intense fear, and sometimes physical reactions such as screaming or thrashing. PTSD nightmares, however, involve vivid recollections of past trauma and occur during REM sleep.
How Does Obstructive Sleep Apnea Influence PTSD Nightmares?
Obstructive sleep apnea (OSA) can exacerbate PTSD nightmares by causing repeated interruptions in breathing during sleep, leading to more fragmented and lighter sleep stages. According to Cleveland Clinic, these frequent awakenings can increase the likelihood of nightmares.
This reduces the ability to enter deep, restorative sleep, ultimately worsening PTSD-related sleep symptoms and impairing overall health outcomes.
Are PTSD Nightmares More Common in Military Personnel?
PTSD nightmares are notably more prevalent among military personnel due to their high exposure to traumatic events during combat. A report from U.S. Department of Veterans Affairs shows that the prevalence of PTSD-related nightmares is significantly higher in veterans compared to the general population.
These nightmares can be particularly distressing, often contributing to the development of chronic sleep issues, including insomnia and REM sleep behavior disorder.
How Can Cognitive Therapy Help With PTSD-Induced Sleep Problems?
Cognitive therapy aims to address the thoughts and beliefs that contribute to PTSD-induced sleep problems, such as fears about sleep and hypervigilance at night. Mayo Clinic describes how cognitive restructuring helps individuals challenge distorted thoughts.
This process helps them develop healthier sleep patterns, reducing the frequency and severity of both nightmares and general sleep disturbances related to PTSD.




